Enhancing Hospital Emergency Readiness and Disaster Management Protocols
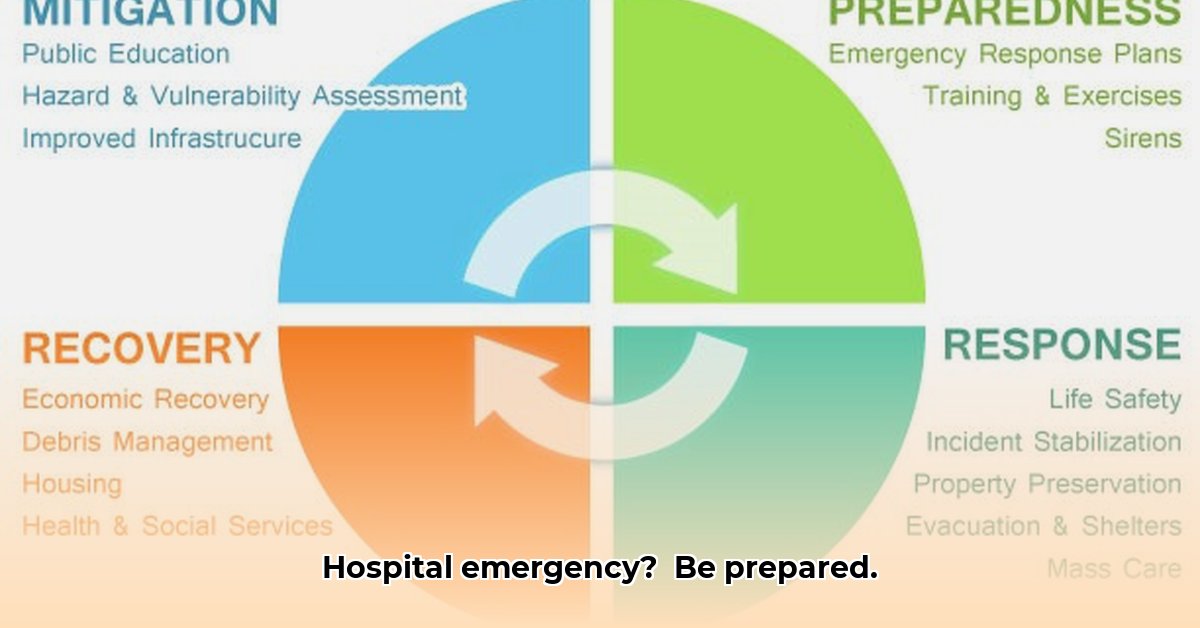
Hospitals must maintain unwavering care during crises like earthquakes, widespread illnesses, or cyberattacks. This guide assists hospitals in developing robust emergency plans that address common pitfalls, offering step-by-step solutions for effective preparation. It provides practical advice to create easily updated plans that safeguard patients, staff, and facilities, serving as a key resource for establishing long-term hospital protection. For information on healthcare coverage, see details here.
Understanding Your Emergency Operations Plan
A robust Emergency Operations Plan (EOP) acts as a hospital’s strategic asset during crises, serving as a guide to ensure smooth operations and protect patient safety amid unexpected events, from natural disasters to pandemics. Without a comprehensive EOP, situations can quickly become chaotic, potentially endangering patients and disrupting essential services. The strength of an EOP lies in transforming chaos into a well-managed scenario. Does your hospital have the necessary preparation in place to handle both predictable emergencies and low-probability, high-impact events?
Six Key Elements for a Successful Emergency Operations Plan
The Joint Commission, a leading healthcare accreditation body, establishes standards for exceptional hospital emergency protocols, highlighting six critical areas that form the foundation of a resilient EOP:
-
Communication: Maintaining Critical Connections: Maintaining clear and redundant communication channels is essential. Hospitals should implement multiple communication methods, such as mass notification systems, two-way radios, satellite phones, and designated communication officers. Regularly test these systems under simulated emergency conditions to ensure reliability and identify weaknesses, preventing failures during actual crises. Document all communication attempts and logs meticulously.
-
Resources and Assets: Strategic Allocation: Effective management of resources like medical supplies, pharmaceuticals, personal protective equipment (PPE), specialized equipment (ventilators, dialysis machines), and personnel is critical during emergencies. Proactive planning should encompass detailed inventory management, just-in-time (JIT) delivery protocols, and mutual aid agreements with neighboring facilities. Consider resource sharing platforms to optimize distribution during widespread events. Conduct regular inventory audits and track expiration dates to minimize waste.
-
Safety and Security: Protecting Patients and Staff: Prioritize patient and staff safety by creating comprehensive evacuation plans, robust security measures, and hazardous material protocols. The goal is to protect lives by adhering to established regulations and best practices. Designate secure areas for sheltering-in-place, and implement access control measures to prevent unauthorized entry. Provide regular training on de-escalation techniques and active shooter response protocols.
-
Staff Responsibilities: Ensuring Team Readiness: Clearly defined roles and responsibilities are necessary for team members to effectively coordinate and avoid confusion. Develop detailed job action sheets for each staff position, outlining specific duties during various emergency scenarios. Implement a credentialing system to verify the qualifications of all responders. Provide cross-training opportunities to enhance staff flexibility and preparedness.
-
Utilities Management: Maintaining Essential Services: Maintaining essential utilities—power, water, HVAC, and communication—is essential, with backup systems in place for potential disruptions. Establish protocols for managing utility failures, including generator testing, water conservation strategies, and alternative communication methods. Implement energy-efficient practices to reduce strain on resources during prolonged events.
-
Clinical and Support Activities: Sustaining Patient Care: Sustaining patient care requires establishing clear procedures for managing patient surges, providing alternative treatment locations, and ensuring continuity of critical services. Develop protocols for triage, patient tracking, and infection control. Establish partnerships with community-based organizations to provide support services, such as transportation, childcare, and mental health counseling.
Risk Assessment: Spotting Trouble Before It Hits
A thorough risk assessment is fundamental to any effective emergency plan, identifying potential hazards and assessing their likelihood and impact. Use a Hazard Vulnerability Analysis (HVA) to prioritize threats and develop mitigation strategies.
| Technology/System | Likelihood of Failure | Impact of Failure | Mitigation Strategies |
|---|---|---|---|
| Communication Systems | Medium | High | Redundant systems (satellite phones, two-way radios), regular testing (bi-weekly drills), alternative communication methods (runners, pre-arranged meeting points) |
| Power Generation | Medium | High | Backup generators (multiple units), fuel storage (sufficient for 96 hours of operation), power purchase agreements with local utilities |
| Water Supply Systems | Low | Medium | Water storage tanks (sufficient for 72 hours of operation), emergency water sources (wells, cisterns), water purification systems (portable filtration units) |
| IT Infrastructure | Medium | High | Data backups (offsite, cloud-based), offsite servers (mirrored data centers), cybersecurity measures (firewalls, intrusion detection systems), IT disaster recovery plan (tested annually) |
| Medical Supply Chains | High (during crises) | High | Diversified suppliers (multiple vendors), emergency stockpiles (essential medications, PPE), strong contracts (guaranteed delivery clauses), supply chain diversification strategies (local sourcing options) |
Actionable Steps: What to Do Now and Later
An EOP requires continuous attention rather than a one-time setup. It should be a living document, regularly updated and practiced.
Short-Term Actions (0-1 Year):
- EOP Review and Gap Analysis: Review your current EOP against the Joint Commission’s standards, FEMA guidelines, and relevant local regulations. Conduct a gap analysis to identify areas for improvement and update accordingly.
- Drills and Exercises: Conduct a variety of drills and exercises (tabletop, functional, full-scale) to assess preparedness and improve plans based on lessons learned. Include scenarios that simulate various types of emergencies, including mass casualty events, cyberattacks, and natural disasters.
- Staff Training: Ensure all staff members are knowledgeable about the EOP, their roles, and emergency procedures. Provide regular training sessions, including hands-on practice and simulations. Implement a competency-based training program to track staff proficiency.
Long-Term Actions (3-5 Years):
- Threat Monitoring and Plan Updates: Continuously monitor potential emergencies, emerging threats, and changes in regulations to update the EOP as needed. Conduct an annual review of the EOP, involving stakeholders from various departments.
- Infrastructure Investment: Invest in resilient infrastructure systems like backup power, reliable water sources, and secure communication networks. Explore opportunities for energy efficiency and sustainable practices to reduce reliance on external resources.
- Community Collaboration: Establish strong communication plans with local organizations, emergency responders, and community stakeholders. Participate in regional emergency planning initiatives and exercises.
- Advanced Training and Certification: Provide advanced training and certification opportunities for key personnel in areas such as incident command, hazardous materials response, and medical surge management.
Working Together: A Team Effort
Effective emergency preparation involves collaboration between hospital leaders, healthcare professionals, government agencies, and community members. According to FEMA (Federal Emergency Management Agency), this collaborative approach facilitates efficient resource sharing and unified responses during crises. Building resilience requires a shared commitment to preparedness. Establish memorandums of understanding (MOUs) with partner organizations to formalize roles and responsibilities.
How to Optimize Hospital Emergency Operations Plans for Low Probability High Impact Events
Key Takeaways:
- Comprehensive Emergency Operations Plans (EOPs) are vital for all healthcare facilities to ensure resilience during unforeseen events.
- Optimizing hospital emergency operations plans for low probability, high impact events requires a proactive, multi-faceted approach encompassing risk assessment, scenario planning, and resource management.
- Regular reviews and updates of EOPs are essential to address emerging threats and adapt to changing circumstances.
- Collaboration among stakeholders, including healthcare facilities, government agencies, and community organizations, is key to effective preparedness.
- Addressing health disparities in preparedness is crucial to ensure equitable access to care during emergencies.
- Technology integration requires robust cybersecurity measures to protect sensitive data and maintain operational functionality.
Understanding Low Probability, High Impact Events
Consider unlikely but devastating events like major pandemics (more lethal strains), cyberattacks (nation-state sponsored), or catastrophic natural disasters (earthquakes above magnitude 9). These are low probability, high impact (LPHI) events, which pose unique challenges due to their infrequency and unprecedented scale. Still, the potential devastation that can occur is high, disrupting operations and causing significant harm. These events often require responses exceeding typical emergency management capabilities.
Building a Robust EOP for LPHI Events
Developing an effective EOP requires more than just compliance. It demands innovative strategies and a willingness to challenge conventional assumptions.
-
Comprehensive Risk Assessment: Begin with a detailed hazard vulnerability analysis (HVA). Don’t just focus on common occurrences; identify LPHI scenarios specific to your hospital’s location, infrastructure, and patient population. Consider the cascading effects and how one event could trigger others (e.g., a cyberattack leading to a loss of power and communication). Utilize advanced modeling techniques to simulate the potential impacts of LPHI events.
-
Scenario Planning: Create detailed scenarios for each identified LPHI event. Evaluate the potential impacts, including patient care disruptions, staff shortages (due to illness, injury, or fear), supply chain failures (national or global scale), and communication breakdowns (loss of internet or cellular service). Identify what resources would be needed (including specialized equipment, medications, and personnel) and your backup options (including alternative suppliers, mutual aid agreements, and volunteer networks).
-
Resource Allocation: Develop a surge capacity plan, including personnel, equipment, medications, and communication systems. Explore partnerships with other healthcare facilities
- Sectioned Tupperware for Organized Meals and Snacks on the Go - March 7, 2026
- Meal Containers with Dividers Keep Foods Separate and Fresh - March 6, 2026
- Tupperware with Dividers Makes Entertaining Easy and Organized - March 5, 2026