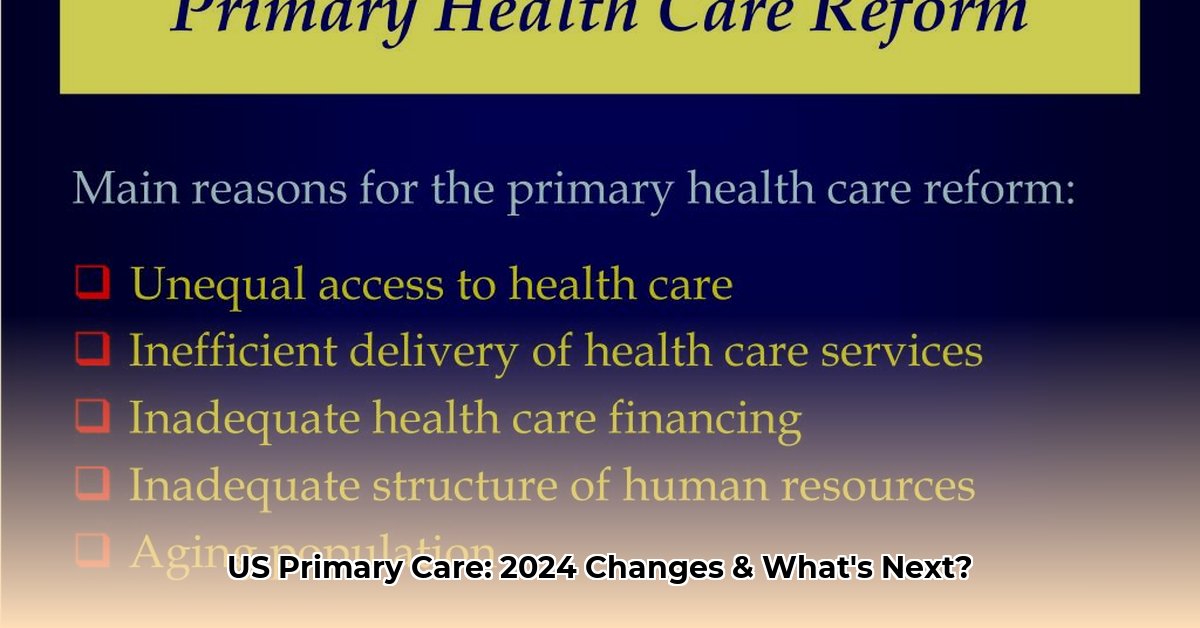
The State of Primary Care: Why Reform Is Necessary
Access to quality primary care is a cornerstone of a healthy population. Yet, the current US primary care system faces significant challenges, hindering its ability to deliver consistent, equitable care. These challenges include rising costs, fragmented services, workforce shortages, and difficulty accessing care, particularly for those in underserved communities. These barriers create disparities, meaning some individuals have a much harder time getting the care they need simply due to their circumstances. This article explores the ongoing efforts to reform primary health care, examining the core issues, innovative solutions being implemented, and the potential impact of these changes.
Reforming the Foundation: Key Initiatives and Goals
Recognizing these challenges, the Department of Health and Human Services (HHS) is leading a comprehensive strategy to reshape primary care. This strategy aims to build a more accessible, equitable, and integrated system, ensuring everyone has the opportunity to achieve their best possible health. Key elements of this strategy include:
- Expanding Insurance Coverage: Broadening insurance coverage is fundamental to making primary care affordable. Increased coverage enables more individuals to seek preventative care without the fear of crippling medical bills.
- Strengthening the Primary Care Workforce: Addressing the shortage of primary care physicians, nurses, and other healthcare professionals is critical. The HHS is investing in training and recruitment programs, aiming to attract and retain skilled professionals, especially in underserved areas. This includes initiatives like loan forgiveness programs to alleviate the financial burden of medical education and efforts to create more reasonable workloads and improve working conditions to prevent burnout.
- Promoting Value-Based Care: Shifting from a fee-for-service model to value-based care is a core component of the HHS strategy. Value-based care rewards providers for positive patient outcomes and efficient care delivery, incentivizing quality over quantity. This transition involves developing effective metrics to measure “value” and ensuring providers are fairly compensated for keeping patients healthy, rather than just treating illness.
- Integrating Behavioral Health: Recognizing the interconnectedness of physical and mental health, the HHS is working to integrate behavioral health services into primary care settings. This integrated approach allows patients to address both their physical and mental health needs in a coordinated manner, improving overall well-being and reducing stigma associated with seeking mental health care.
- Harnessing Technology: The HHS is actively exploring the potential of technology, particularly telehealth, to expand access to care. Telehealth offers a convenient way for patients, especially those in rural or underserved areas, to connect with healthcare providers. While in-person visits remain essential, telehealth can bridge geographical gaps and improve access for individuals with mobility challenges or limited transportation options.
Addressing Current Challenges in Primary Care
The path to primary care reform requires tackling several key obstacles:
- Outdated Payment Models: The traditional fee-for-service model often incentivizes unnecessary tests and procedures. The transition to value-based care, while promising, presents challenges in defining and measuring “value” and ensuring fair provider reimbursement.
- Access Disparities: Significant disparities in access to primary care exist, particularly in rural and underserved communities. These disparities lead to delayed diagnoses, increased reliance on emergency rooms, and poorer health outcomes. Solutions like telehealth and mobile clinics offer some promise, but addressing the underlying causes of these disparities requires comprehensive, community-based strategies.
- Workforce Shortages: The shortage of primary care professionals is a growing crisis, driven by factors like high medical education debt, burnout, and lower pay compared to specialized fields. Addressing this shortage requires a multi-pronged approach, including loan forgiveness programs, improved working conditions, and increased recognition of the vital role primary care plays in our healthcare system.
- Technology Limitations: While electronic health records (EHRs) hold potential, current systems often suffer from usability issues, lack of interoperability, and contribute to administrative burdens. Improving EHR interfaces, enhancing interoperability, and increasing automation could free up valuable time for patient care.
- Policy and Regulatory Hurdles: Navigating complex regulations and reporting requirements adds to the administrative burden on primary care practices. Streamlining these processes and reducing unnecessary paperwork could allow providers to focus more on patient care.
- Shifting Perspectives: A historical overemphasis on specialty care has contributed to a fragmented and expensive healthcare system. Reforming primary care requires a shift in perspective, recognizing its importance as the foundation of a healthy population and investing accordingly.
New Payment and Delivery Models
The shift towards value-based care is driving innovation in payment and delivery models:
- Accountable Care Organizations (ACOs): These networks of providers share responsibility for coordinating care for a defined patient population, sharing in cost savings when they improve quality and efficiency.
- Patient-Centered Medical Homes (PCMHs): These models emphasize comprehensive, coordinated care led by a primary care physician, focusing on individual patient needs and fostering strong patient-doctor relationships.
- Bundled Payments: These single payments cover an entire “episode of care,” such as a surgery, incentivizing providers to collaborate and reduce costs.
- Pay-for-Performance (P4P): These programs reward providers for achieving specific performance targets related to quality and efficiency.
The Centers for Medicare & Medicaid Services (CMS) and professional organizations like the American Academy of Family Physicians (AAFP) offer resources and support to providers transitioning to these new models.
The Future of Primary Care
Transforming primary care is an ongoing journey. While challenges remain, the shift toward value-based care, coupled with investments in the workforce, technology, and community partnerships, offers hope for a more equitable, accessible, and effective primary care system. Ongoing research and evaluation are crucial to understanding the impact of these reforms and adapting strategies to meet evolving needs. The likely future of primary care involves greater integration of technology, addressing social determinants of health, and a renewed focus on preventative care. While the path ahead is complex, the pursuit of a patient-centered, high-quality primary care system for all remains a priority.
- Rectangular Glass Food Storage Containers For Meal Prep - January 27, 2026
- Borosilicate Glass Food Containers Keep Meals Fresh and Organized - January 26, 2026
- Choosing Glass Containers With Snap Lids for Fresh Food Storage - January 25, 2026