Delivering quality primary health care is a global challenge, but it’s particularly complex in low-resource settings. This article explores the multifaceted challenges and innovative solutions addressing these critical issues, offering a guide to strengthening primary healthcare systems worldwide.
Understanding the Challenges
Providing essential healthcare in resource-limited environments presents a complex web of interconnected obstacles. Understanding these challenges is crucial for developing effective solutions.
Infrastructure Deficiencies
Many low-resource settings lack basic infrastructure necessary for effective healthcare delivery. Dilapidated buildings, unreliable utilities (like electricity and clean water), and insufficient equipment hinder even the most basic medical procedures, probably contributing to poorer patient outcomes. Improving infrastructure is not merely about constructing new buildings; it involves ensuring reliable access to essential resources.
Funding Gaps and Resource Scarcity
Healthcare services require significant financial investment. In low-resource settings, limited funding creates a ripple effect, impacting everything from staff shortages and inadequate training to the availability of essential medicines and technologies. This financial strain can create a vicious cycle, hindering progress and perpetuating health disparities. Some experts believe that without increased funding, significant improvements are unlikely.
The Healthcare Human Resource Crisis
A shortage of trained healthcare professionals, including doctors, nurses, and midwives, is a widespread problem. Existing staff are often overworked and stretched thin, impacting the quality of care they can provide and likely contributing to burnout. Addressing this crisis requires not only training new healthcare workers but also implementing strategies to retain existing staff.
Supply Chain Disruptions and Logistics
Even when medicines and supplies are available, delivering them to those in need can be problematic. Unreliable transportation networks, inadequate storage facilities (particularly for temperature-sensitive medications and vaccines), and difficult terrain often disrupt the supply chain. These disruptions can lead to expired medications, shortages of essential supplies, and ultimately, compromise patient care. Ongoing research suggests improvements in logistics and infrastructure are essential.
The Double Burden of Disease
Many low-resource areas face the dual challenge of managing both infectious diseases (like malaria, tuberculosis, and HIV/AIDS) and a rising prevalence of non-communicable diseases (NCDs) such as diabetes, heart disease, and cancer. This double burden strains limited resources and requires integrated approaches to care. The WHO’s Package of Essential NCD Interventions (PEN) offers a framework for tackling this complex issue.
Innovative Solutions and Interventions
Despite these daunting challenges, innovative solutions are emerging, offering hope for improved primary healthcare in underserved areas.
Empowering Community Health Workers (CHWs)
CHWs are local individuals trained to provide basic healthcare services and health education within their communities. They serve as a vital link between formal healthcare systems and underserved populations, particularly in remote or hard-to-reach areas. Investing in CHW training and support can significantly expand access to care and promote community ownership of health initiatives.
Leveraging Mobile Health (mHealth)
Mobile technology, including smartphones and tablets, offers unprecedented opportunities to improve healthcare access. mHealth applications can be used for patient education, remote monitoring of chronic conditions, data collection, and communication between healthcare providers and patients. mHealth has the potential to bridge geographical barriers and improve the efficiency of healthcare delivery.
Strengthening Supply Chains
Improving supply chain management is crucial for ensuring that essential medicines and supplies reach those who need them. This involves implementing robust logistics systems, appropriate storage solutions (including temperature-controlled facilities for vaccines and other sensitive medications), and reliable transportation networks. Research suggests that efficient supply chains are fundamental to providing consistent and reliable healthcare services.
Addressing the Double Burden of Disease through Integration
Integrating care for both infectious diseases and NCDs is essential for maximizing resource utilization and improving health outcomes. The WHO PEN framework provides guidance for implementing cost-effective interventions for NCDs, while existing programs for communicable diseases can be adapted and strengthened. Some studies suggest that integrated care models may lead to better patient outcomes and more efficient use of resources.
Financial Innovations for Sustainable Healthcare
Sustainable financing is critical for long-term success. Exploring innovative financing mechanisms, such as micro-insurance schemes, performance-based financing, and public-private partnerships, can help mobilize additional resources and ensure the financial viability of primary healthcare services.
The Role of WHO PEN and Other Frameworks
The WHO PEN framework provides practical guidance for integrating NCD care into primary healthcare services in resource-limited settings. It emphasizes early detection, prompt treatment, and community empowerment. Other frameworks and guidelines, such as those for maternal and child health and communicable diseases, also play a crucial role in guiding primary healthcare delivery. Integrating these frameworks can create a more comprehensive and effective approach to healthcare.
Case Studies and Examples
Highlighting successful programs and initiatives provides valuable insights and demonstrates the feasibility of various interventions. For example, the success of community-based malaria control programs in several African countries showcases the effectiveness of community engagement and ownership. Similarly, the use of mHealth for diabetes management in India demonstrates the potential of technology to improve care in resource-constrained environments.
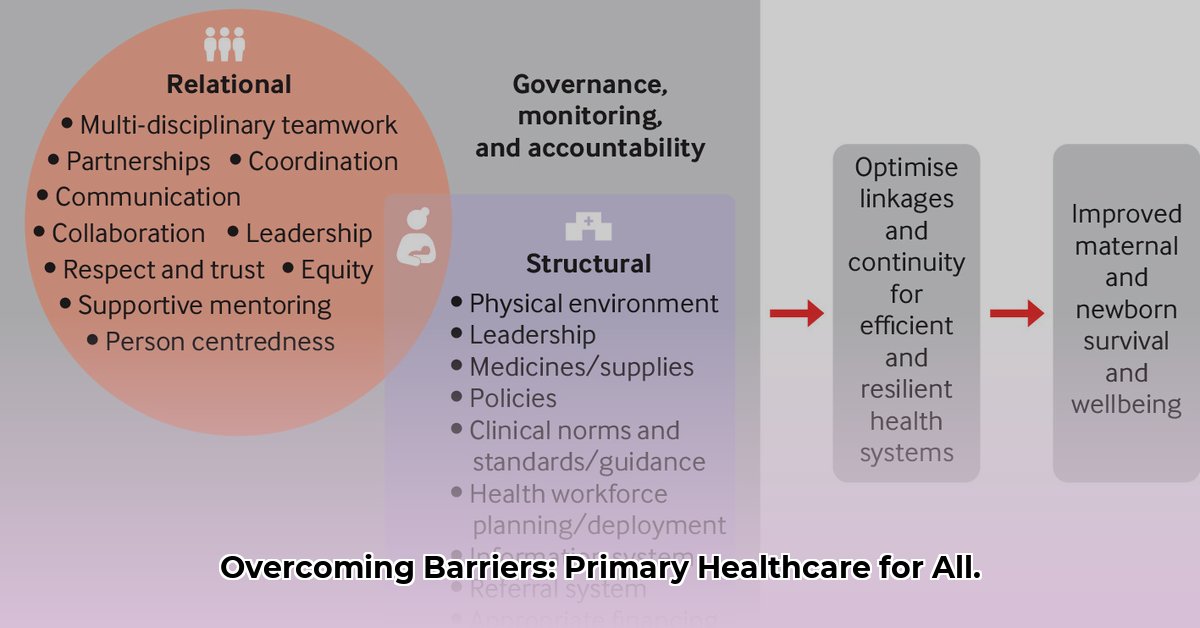
The Importance of Collaboration and Stakeholder Engagement
Strengthening primary healthcare requires a collaborative approach. Governments, NGOs, international organizations, community leaders, and healthcare professionals must work together to ensure sustainable improvements. Engaging local communities in the planning and implementation of healthcare initiatives is crucial for ensuring that services are culturally appropriate and meet the specific needs of the population.
Future Directions and Innovations
The future of primary healthcare in low-resource settings will likely be shaped by ongoing innovation. Emerging technologies, such as artificial intelligence (AI) and point-of-care diagnostics, hold immense potential for improving diagnostics, personalizing treatment, and enhancing healthcare delivery. Integrating climate change considerations into healthcare planning is also becoming increasingly important for building more resilient health systems.
A Call to Action
Improving primary healthcare in low-resource settings is a shared responsibility. Everyone has a role to play, from advocating for increased funding and supporting organizations working on the ground to volunteering time and expertise. By working together and embracing innovation, we can create a healthier and more equitable future for all.
- Divided Food Storage Containers Transform Meal Prep and Portion Control - February 8, 2026
- Divided Food Containers Are Meal Preps Secret Weapon - February 7, 2026
- Food Kits for Adults Offer Fun DIY Cooking Adventures - February 6, 2026