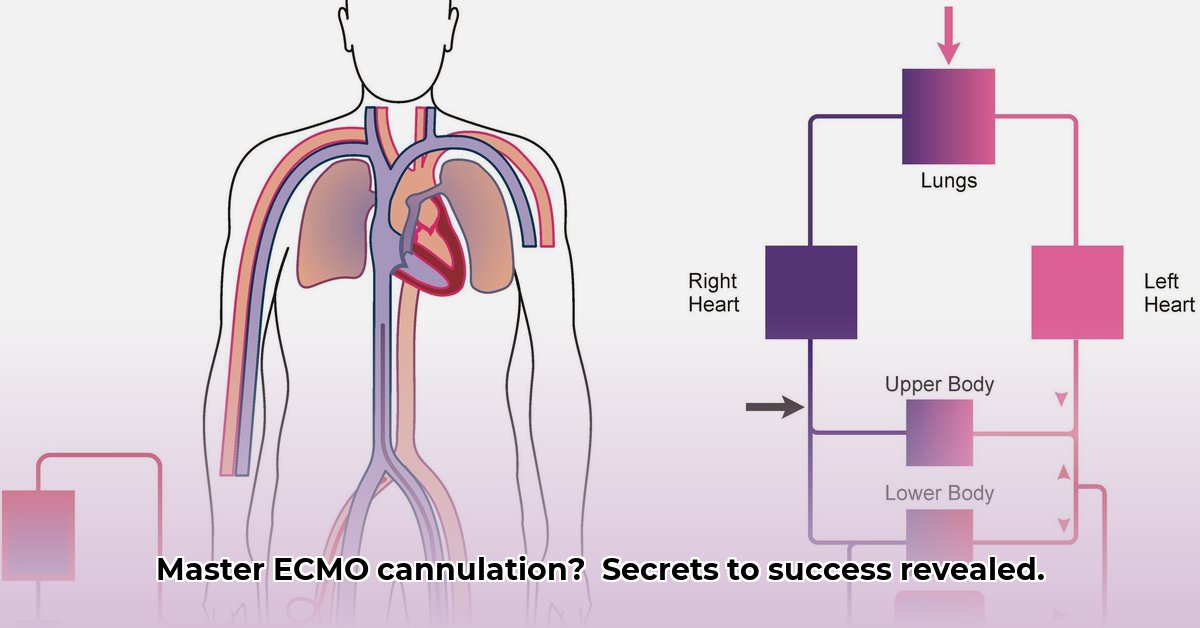
Extracorporeal membrane oxygenation (ECMO) is a life-saving technique that temporarily takes over the function of the heart and lungs. Precise placement of cannulas (tubes) during cannulation is crucial for a patient’s survival and recovery. This article provides a comprehensive overview of ECMO cannulation, comparing methods and highlighting key considerations for healthcare providers of all experience levels to perform ECMO cannulation safely and effectively, ultimately improving patient outcomes.
ECMO Cannulation: A Guide to Best Practices
ECMO cannulation involves inserting cannulas into blood vessels to connect a patient to an extracorporeal life support machine. It is a critical medical procedure requiring precision and skill. A key decision is choosing between peripheral and central cannulation configurations, each offering distinct advantages and disadvantages.
Choosing the Right Approach: Peripheral vs. Central ECMO Access
Selecting the optimal ECMO cannula insertion method depends on several factors, including the urgency of the situation, the patient’s anatomy, and the type of support required.
Peripheral cannulation, which involves placing cannulas in larger blood vessels near the body’s surface, may be favored in urgent situations due to its relative speed and ease of access. Common sites for peripheral cannulation include the femoral artery and vein in the groin, as well as the axillary artery and vein in the armpit. While less invasive than central cannulation, peripheral cannulation may offer less precise blood flow control and is associated with potential complications such as limb ischemia.
Central cannulation involves direct insertion of cannulas into the heart or great vessels, such as the right atrium and aorta. This approach offers more precise blood flow control and can provide greater hemodynamic support. However, central cannulation is a more complex procedure with an increased risk of complications, including bleeding, infection, and injury to surrounding structures. Furthermore, central cannulation typically requires a surgical cutdown, which may not be feasible in all patients.
The type of ECMO support needed (veno-venous (VV) or veno-arterial (VA)), the patient’s body shape, existing health problems, and overall health status should also be considered. This approach prioritizes the unique patient needs. VV ECMO is primarily used for respiratory support, while VA ECMO provides both respiratory and circulatory support. The choice between VV and VA ECMO depends on the patient’s underlying condition and the goals of therapy.
Optimizing ECMO Cannulation: A Step-by-Step Guide
For successful ECMO cannulation, a carefully executed step-by-step process helps minimize risks and optimize outcomes.
- Pre-Cannulation Assessment: Thoroughly assess the patient’s anatomy, blood flow, and coagulation status. Use imaging techniques like ultrasound or fluoroscopy (X-rays) to identify the best blood vessels and prevent complications. Key assessments include echocardiography to evaluate cardiac function and vascular ultrasound to assess vessel size and patency. Cannula size selection depends on patient size and required blood flow.
- The Cannulation Procedure Itself: Strict sterile conditions are crucial. Physicians use imaging guidance to precisely insert cannulas, minimizing damage to surrounding tissues or organs. Avoiding arterial injury or venous obstruction is essential. The Seldinger technique, a percutaneous approach, is commonly used for peripheral cannulation, while open surgical techniques are often employed for central cannulation.
- Post-Cannulation Monitoring: Closely monitor the patient’s blood pressure, oxygen saturation, and coagulation parameters. Regular blood tests help detect potential issues, and ECMO settings are adjusted to provide optimal support. Constant management of these parameters is essential. Monitor for signs of bleeding, infection, and limb ischemia.
- Decannulation (Tube Removal): Carefully remove cannulas under strict sterile conditions when the patient’s condition improves. Continued close monitoring is necessary to detect any immediate problems. Decannulation should be performed by experienced personnel, and hemostasis must be carefully achieved to prevent bleeding complications.
The Challenges: Potential Complications
Possible complications include bleeding, infection, blood clots (thrombosis), air embolism, and damage to nearby organs or nerves. Careful technique, continuous monitoring, and proactive care are vital for preventing these complications. Proactive measures to minimize these risks include meticulous sterile technique, prophylactic antibiotics, and vigilant monitoring for signs of infection. Anticoagulation is essential to prevent thrombosis, but must be carefully managed to avoid bleeding complications.
The Future of ECMO Cannulation: Innovations and Advancements
Ongoing research aims to enhance ECMO cannulation safety and reduce invasiveness. Key goals include developing simpler cannulation techniques, improved cannula designs, and less invasive approaches, along with new tube materials that reduce blood clot formation. Advanced monitoring systems provide real-time data on hemodynamics, improving accuracy and enhancing safety. Developments in biocompatible coatings aim to minimize the inflammatory response associated with ECMO.
Actionable Insights for Healthcare Providers Involved in ECMO Cannulation
The following summarizes key actions for stakeholders in ECMO cannulation:
| Stakeholder Group | Immediate Actions | Long-Term Strategies |
|---|---|---|
| ECMO Teams | Standardize procedures; improve training; utilize checklists; adopt ultrasound guidance. | Conduct further research; create better prediction models; refine techniques; develop protocols for managing specific complications. |
| Hospitals/ICUs | Invest in better imaging equipment; establish dedicated ECMO units; ensure adequate staffing. | Support better reporting standards; fund research and development; promote interdisciplinary collaboration. |
| Device Manufacturers | Improve cannula design; use better materials; develop better sensors; enhance biocompatibility. | Invest in less invasive techniques; develop advanced materials; explore novel monitoring technologies. |
| Regulatory Bodies | Create certification programs; update guidelines; promote standardization. | Support international collaboration; work towards global ECMO standards; establish quality metrics for ECMO centers. |
Mastering ECMO cannulation requires a lifelong commitment to best practices, meticulous execution, and dedication to continuous learning and improvement. Addressing potential complications proactively and embracing new technologies is essential for improving patient outcomes and using this life-saving technology effectively.
How to Select Optimal ECMO Cannulation Sites Based on Patient Characteristics
Key Takeaways:
- Patient-specific factors are paramount in choosing ECMO cannulation sites.
- Ultrasound guidance is crucial for precise cannula placement, minimizing complications.
- Minimizing recirculation and maintaining adequate blood flow are key objectives.
- The choice between veno-venous (VV) and veno-arterial (VA) ECMO depends on the primary organ failure.
- Hybrid configurations offer flexibility to address limitations of standard approaches.
- Careful consideration of cannula size, type, and placement is essential to optimize ECMO effectiveness and minimize complications such as thrombosis and differential hypoxemia (low blood oxygen).
Understanding the Decision-Making Process
Selecting the ideal ECMO cannulation site involves carefully weighing patient characteristics and anticipated clinical needs. Age, weight, underlying health conditions, and the severity of organ failure are key variables that impact the effectiveness and safety of ECMO support. Patient assessment must include a thorough evaluation of cardiovascular, respiratory, and neurological function.
Key Patient Characteristics to Consider
Several patient characteristics influence how to select optimal ecmo cannulation sites based on patient characteristics. These factors often guide the choice between femoral ECMO (using femoral vein/artery) and jugular approaches ECMO (using veins in the neck), or even dictate the need for a hybrid strategy.
- Age and Size: Infants and young children frequently require jugular cannulation due to smaller vessel sizes in the femoral region. Adults often readily tolerate femoral access. Weight significantly impacts cannula size selection and influences the overall hemodynamic response to ECMO. Cannula size is typically determined based on body surface area (BSA) and desired blood flow rates.
- Underlying Conditions: Existing vascular disease, prior surgeries affecting vascular access, or coagulopathies (blood clotting disorders) can significantly impact cannulation site selection. Previous femoral artery procedures might make jugular cannulation more preferable. Thorough review of the patient’s medical history and physical examination is essential to identify potential contraindications to cannulation at specific sites.
- Severity of Illness: The severity of respiratory or cardiac failure directly impacts the urgency of cannulation. In life-threatening situations, readily accessible femoral sites might be prioritized over jugular access, which requires more extensive preparation. The need for immediate circulatory support may necessitate VA ECMO with rapid femoral cannulation.
- Expected Duration of ECMO: For shorter ECMO runs, femoral access is often chosen for its ease and speed of cannulation. Longer durations, however, might necessitate jugular cannulation to minimize infection risks and allow for greater patient mobility. Prolonged femoral cannulation is associated with increased risk of vascular complications, such as deep vein thrombosis.
Cannulation Site Options: A Comparative Overview
The two most common approaches are femoral and jugular cannulation. Each has its own strengths and weaknesses:
| Cannulation Site | Advantages | Disadvantages |
|---|---|---|
| Femoral | Relatively easy access; rapid cannulation; good patient mobility (initially); can be performed percutaneously; allows for large cannula size. | Higher risk of bleeding; potential for vascular complications (e.g., thrombosis, limb ischemia); can limit mobility with longer runs; retrograde arterial flow in VA ECMO. |
| Jugular | Lower risk of bleeding complications; improved patient comfort with |
- Sectioned Tupperware for Organized Meals and Snacks on the Go - March 7, 2026
- Meal Containers with Dividers Keep Foods Separate and Fresh - March 6, 2026
- Tupperware with Dividers Makes Entertaining Easy and Organized - March 5, 2026