Unequal Impacts: Chronic Diseases and Disparities
Chronic diseases—like heart disease, diabetes, and cancer—pose a significant challenge in the United States, but their impact isn’t felt equally across all populations. Certain groups face a disproportionately higher risk of developing these diseases, often due to systemic inequities rather than individual choices. This article explores the complex interplay of social, economic, and environmental factors that contribute to these disparities, highlighting specific diseases and offering potential solutions for a healthier, more equitable future.
Unmasking Health Inequities: What Are They and Why Do They Exist?
Health inequities aren’t simply differences in health outcomes; they are avoidable disparities rooted in systemic issues. For example, unequal access to quality healthcare, nutritious food, and safe environments can lead to drastically different health outcomes, even for individuals with the same underlying health conditions. These inequities often stem from social determinants of health – the conditions in which we live, work, and age.
Key Social Determinants of Health:
- Socioeconomic Factors: Poverty and limited education can restrict access to healthy resources and hinder informed decision-making. Someone struggling to afford basic necessities may find it challenging to prioritize preventive care or healthy eating.
- Neighborhood and Environment: Unsafe neighborhoods, limited access to fresh food (food deserts), and exposure to environmental hazards like pollution all increase the risk of chronic diseases.
- Discrimination: Experiences of racism, sexism, and other forms of discrimination can contribute to chronic stress and limit opportunities, negatively impacting both physical and mental health.
- Healthcare Access: Lack of health insurance or access to quality medical care hinders early diagnosis and treatment, potentially worsening existing health problems. This is especially critical for managing chronic conditions that require ongoing care.
These factors are interconnected and can create a cumulative effect, increasing the likelihood of chronic diseases for certain populations.
Which Chronic Diseases are Most Affected by Health Inequities?
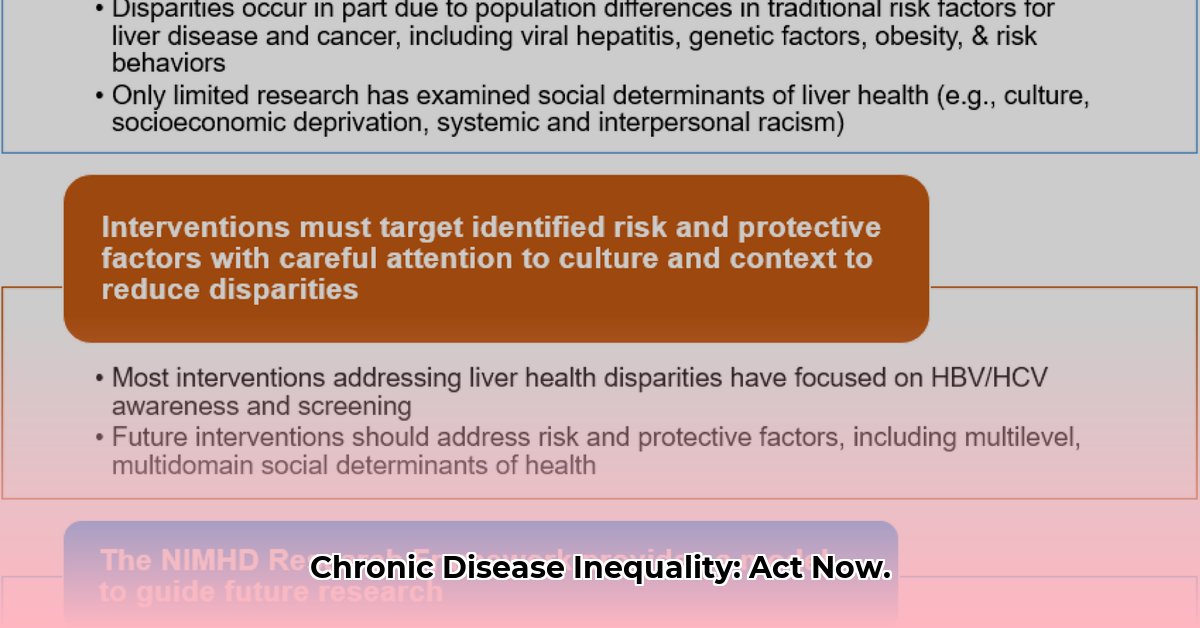
Several chronic diseases exhibit stark disparities across different populations. These differences aren’t solely due to genetics; they’re deeply intertwined with social and economic factors.
- Diabetes: Rates are significantly higher among Native Americans, African Americans, and Hispanic/Latinx populations. This may be partially attributed to limited access to nutritious food, culturally appropriate education programs, and consistent healthcare.
- Heart Disease: African Americans experience disproportionately higher rates of heart disease, potentially due to factors like systemic racism, limited access to quality care, and socioeconomic disadvantages.
- Certain Cancers: Incidence and mortality rates for specific cancers vary significantly across racial and ethnic groups, reflecting disparities in access to screening, treatment, and other resources.
These examples illustrate how social determinants contribute to unequal health outcomes. Two individuals with similar genetic predispositions to heart disease may experience vastly different outcomes depending on their access to resources and their social environment. Someone living in a neighborhood with safe parks, access to healthy food, and readily available healthcare has a clear advantage over someone lacking these resources.
Who is Most at Risk?
Health inequities disproportionately impact vulnerable populations, including:
- People living in poverty: Financial constraints can limit access to healthy food, healthcare, safe housing, and other essential resources.
- Racial and ethnic minorities: Systemic racism and discrimination can lead to reduced opportunities and increased exposure to health risks.
- People with disabilities: Navigating the healthcare system and accessing necessary resources can present significant challenges.
- Rural communities: Limited access to healthcare providers and healthy food options are common barriers.
- Older adults: Age-related health challenges are often compounded by social and economic vulnerabilities.
These groups often face multiple, intersecting challenges that increase their risk of chronic diseases and limit their access to effective prevention and treatment.
Root Causes and Consequences of Health Inequities
The root causes of health disparities are multifaceted and include:
- Limited Healthcare Access: Difficulty affording medications, lack of transportation to appointments, and language barriers can hinder access to quality care.
- Socioeconomic Disadvantage: Poverty limits access to nutritious food, safe housing, and quality education, contributing to poor health outcomes.
- Environmental Injustice: Exposure to pollution, lack of green spaces, and unsafe neighborhoods disproportionately affect marginalized communities.
- Structural Racism and Discrimination: Systemic inequities create barriers to opportunity and resources, negatively impacting health outcomes for certain groups.
These factors contribute to a cycle of disadvantage, perpetuating health disparities across generations. The consequences are far-reaching, impacting not only individual health but also the broader community and healthcare system. Increased healthcare costs, reduced workforce productivity, and widening social inequalities are just some of the consequences of unaddressed health disparities.
What Can We Do? Potential Solutions and Ongoing Research
Tackling health inequities requires a comprehensive approach that addresses both the root causes and the immediate consequences. Potential solutions include:
- Investing in Underserved Communities: Improving access to education, affordable housing, healthy food, and safe environments can make a profound difference.
- Promoting Health Equity Through Policy Changes: Policies that address systemic discrimination, expand access to affordable healthcare, and increase funding for community health centers are essential.
- Empowering Communities: Supporting community-led programs that address local needs and build resilience can be highly effective.
- Culturally Competent Healthcare: Healthcare providers need training and resources to provide culturally sensitive care that respects and understands the unique needs of diverse populations.
- Ongoing Research and Data Collection: Continued research is crucial to understand the complex interplay of factors influencing health disparities and to develop targeted interventions. Some researchers suggest focusing on early childhood interventions, while others emphasize the importance of addressing structural racism and other systemic inequities.
Addressing health inequities is not merely a social justice issue; it’s a public health imperative. By working collaboratively to address the root causes of these disparities, we can create healthier, more equitable communities for everyone. The pursuit of health equity requires ongoing effort, research, and a commitment to dismantle systemic barriers to health and well-being.
- Rectangular Glass Food Storage Containers For Meal Prep - January 27, 2026
- Borosilicate Glass Food Containers Keep Meals Fresh and Organized - January 26, 2026
- Choosing Glass Containers With Snap Lids for Fresh Food Storage - January 25, 2026