Unveiling Health Inequities: A Data-Driven Perspective
This report examines health disparities within the United States, using the most recent available data. By exploring key indicators such as mortality rates, disease prevalence, and access to care, we aim to provide a clear, objective picture of health inequities across different demographic groups.
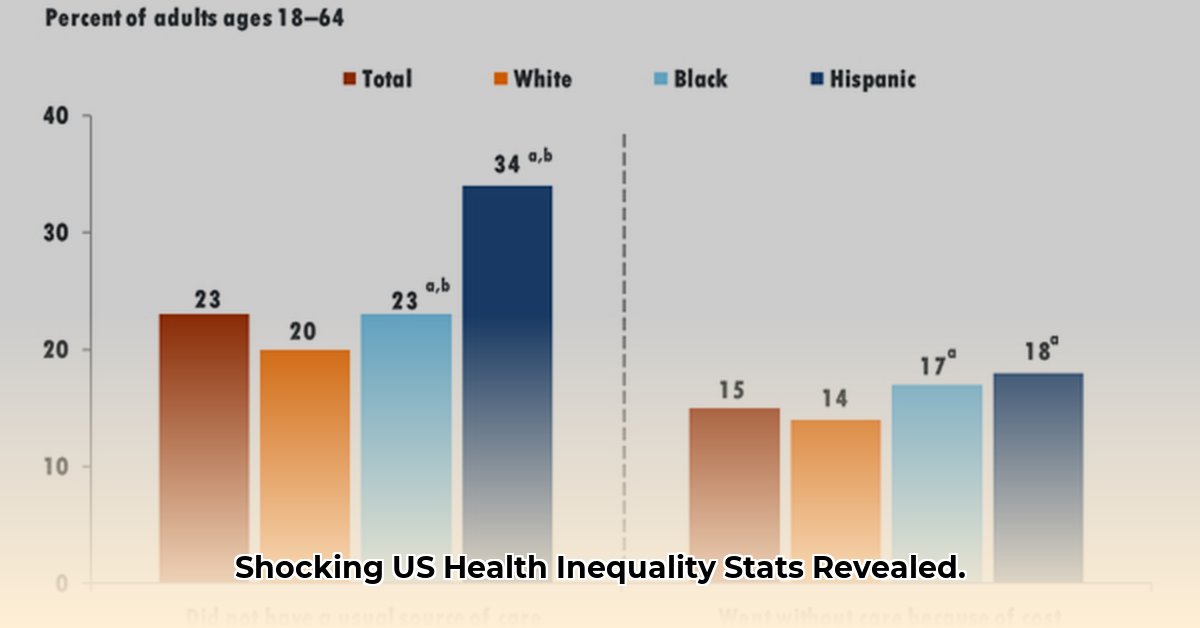
Access to Healthcare: Unequal Opportunities
Access to healthcare, including insurance coverage and timely medical services, remains unevenly distributed. Data from 2022 (KFF, 2024) indicates that 19% of American Indian/Alaska Native (AIAN) adults lacked health insurance, compared to 7% of White adults. Disparities were also evident among Hispanic adults, with 18% uninsured. These discrepancies likely contribute to disparities in preventative care and disease management.
Mental Health: Unequal Burdens
Mental health disparities reveal significant gaps in access to and utilization of mental health services. In 2022 (NIMH, 2024), an estimated 56% of White adults with mental illness received treatment, compared to 38% of Black adults, 40% of Hispanic adults, and 36% of Asian adults. Several factors, including cultural stigma and limited access to culturally competent mental health providers, may contribute to these disparities.
Preventive Care: Disparities in Flu Vaccination
Flu vaccination rates highlight further disparities in preventative care. During the 2022-2023 flu season (CDC, 2024), vaccination rates lagged among minority groups: 63% of Hispanic adults, 63% of AIAN adults, and 58% of Black adults did not receive a flu shot, compared to 49% of White adults. Factors such as access to vaccination sites and mistrust of the healthcare system may influence these differences.
Life Expectancy and Mortality: Stark Realities
Life expectancy, a key indicator of overall health, reveals stark disparities. Preliminary 2022 data (NCHS, 2024) suggests life expectancy for AIAN individuals was approximately 68 years, and for Black individuals, approximately 73 years, compared to approximately 78 years for White individuals. Infant mortality rates also reflect deep inequities. In 2022 (NCHS, 2024), the infant mortality rate for Black infants was 10.9 deaths per 1,000 live births, nearly two and a half times the rate for White infants (4.5). AIAN infants also experienced a disproportionately high rate of 9.1 deaths per 1,000 live births.
Food Insecurity: Unequal Access to Nutrition
Food insecurity, the lack of consistent access to adequate food, disproportionately affects minority children. In 2022 (USDA, 2024), 24% of AIAN children, 21% of Black children, and 15% of Hispanic children experienced food insecurity, compared to 6% of White children.
Summary of Key Health Disparities Indicators (2022)
| Health Indicator | White | Black | Hispanic | AIAN |
|---|---|---|---|---|
| Lack of Health Insurance | 7% | – | 18% | 19% |
| Mental Health Services Received | 56% | 38% | 40% | 36% |
| Flu Vaccination Rate (2022-2023) | 49% | 58% | 63% | 63% |
| Life Expectancy | 78 yrs | 73 yrs | – | 68 yrs |
| Infant Mortality Rate | 4.5 | 10.9 | – | 9.1 |
| Child Food Insecurity Rate | 6% | 21% | 15% | 24% |
Note: Data for certain indicators are not available for all racial/ethnic groups. “-” indicates missing data.
The Complexities of Health Disparities: A Deeper Dive
While the 2022 data provides a valuable snapshot, understanding health disparities requires ongoing analysis. Several factors contribute to these persistent inequities, including social determinants of health, systemic racism, and access to quality healthcare.
Social Determinants of Health: Shaping Health Outcomes
Social determinants, such as income, education, housing, and neighborhood environment, significantly influence health outcomes. Research suggests that individuals living in poverty, with limited educational opportunities, or in areas with poor environmental conditions may experience higher rates of chronic diseases and lower life expectancies. For example, limited access to healthy food options can contribute to higher rates of obesity and diabetes, while inadequate housing can exacerbate respiratory illnesses.
Systemic Racism: A Persistent Barrier
Systemic racism embedded within social structures and institutions creates barriers to healthcare access, quality of care, and positive health outcomes for people of color. Studies have documented how racial bias among healthcare providers can lead to misdiagnosis, inadequate treatment, and lower adherence to medical recommendations. Addressing systemic racism requires comprehensive policy changes and cultural shifts within the healthcare system and society as a whole.
Access to Quality Healthcare: A Fundamental Right
Unequal access to quality healthcare services, including preventative care, diagnostic testing, and treatment, further contributes to health disparities. Individuals lacking health insurance or facing financial barriers to care may postpone or forgo necessary medical attention, potentially leading to worsening health conditions and poorer outcomes.
The Path Forward: Addressing Health Inequities
Addressing health disparities requires multi-pronged strategies focused on both immediate interventions and long-term systemic changes. Current research suggests several promising avenues:
- Improving Access to Quality Healthcare: Expanding health insurance coverage, increasing the availability of culturally competent healthcare providers, and reducing financial barriers to care are essential steps toward ensuring that everyone has access to the healthcare they need.
- Addressing Social Determinants of Health: Investing in programs that improve education, housing, food security, and neighborhood safety can create healthier environments and promote positive health outcomes.
- Combating Systemic Racism: Dismantling systemic racism within healthcare and broader society requires ongoing efforts to address implicit bias, promote diversity and inclusion, and create equitable policies.
- Investing in Research and Data Collection: Continued research on health disparities is crucial for understanding the complex interplay of factors that contribute to these inequities and identifying effective interventions.
By acknowledging the complex interplay of these factors and committing to evidence-based solutions, we can strive toward a more equitable healthcare system and improve health outcomes for all.
Key Statistics on Mortality, Disease Prevalence, and Access to Care (2023)
| Demographic Group | Life Expectancy | Leading Cause of Death | Prevalence of Diabetes | Health Insurance Coverage | Access to Preventative Care (e.g., Flu Vaccine) |
|---|---|---|---|---|---|
| White | 76.9* | Heart Disease | 8.0%* | 92.3%* | 57.0%* |
| Black | 70.8* | Heart Disease | 12.5%* | 84.8%* | 48.3%* |
| Hispanic/Latinx | 77.6* | Cancer | 11.8%* | 79.5%* | 51.3%* |
| *Source: 2023 National Healthcare Quality and Disparities Report |
Note: This table presents a simplified view of complex data. The leading cause of death and prevalence of diabetes may vary within these broad demographic categories. Further research is encouraged for a more nuanced understanding.
- Borosilicate Containers Keep Food Fresh and Your Kitchen Organized - January 24, 2026
- Borosilicate Glass Storage Containers Handle Extreme Temperatures Safely - January 23, 2026
- Borosilicate Glass Food Storage Containers Bring Durable Safety To Your Kitchen - January 22, 2026