Primary Health Care (PHC) is the bedrock of Universal Health Coverage (UHC), ensuring everyone, everywhere can access quality health services without financial hardship. Championed by the World Health Organization (WHO), PHC represents a holistic approach to health, addressing individual needs throughout life. This comprehensive guide explores the principles, implementation, and impact of WHO PHC, offering insights into its crucial role in achieving global health and well-being.
Understanding the Core of PHC
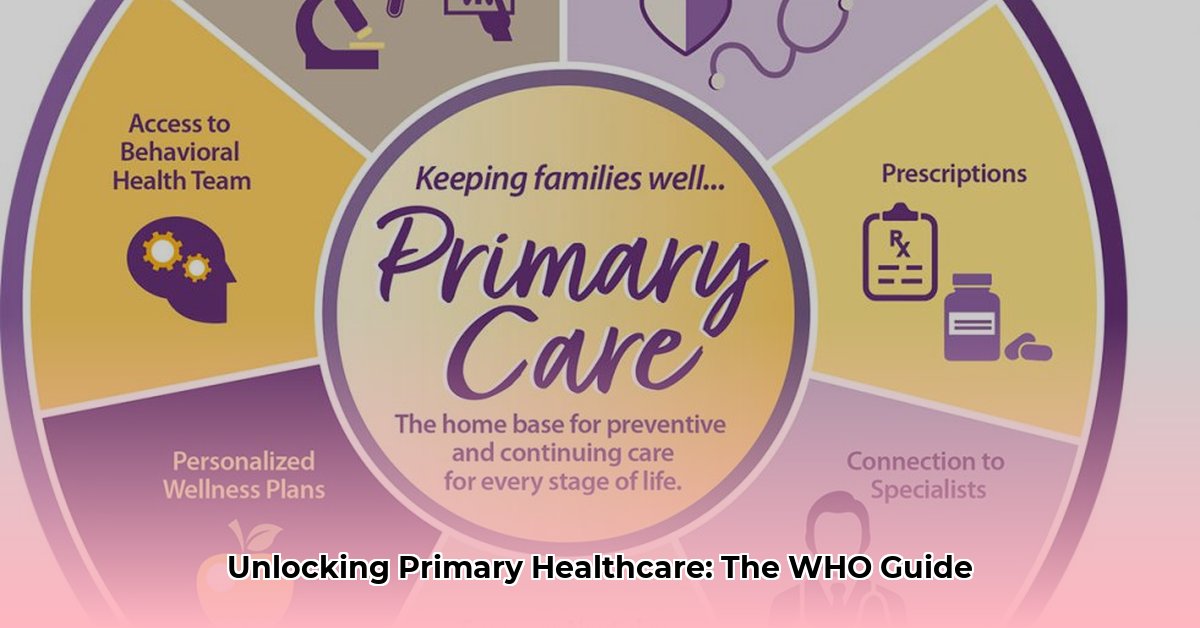
PHC isn’t merely about treating illness; it’s about fostering well-being and empowering individuals and communities. It tackles social, economic, and environmental factors influencing health, moving beyond simply providing medical care. The WHO defines PHC as a whole-of-society approach, aiming for the highest possible level of health and well-being for all. This involves focusing on people’s needs across the health continuum – from promotion and prevention to treatment, rehabilitation, and palliative care.
Three interlinked components form the foundation of WHO PHC:
-
Integrated Health Services: Centered around primary care and essential public health functions, these services ensure individuals receive comprehensive care throughout their lives. This may include vaccinations, health screenings, chronic disease management, and more.
-
Multi-sectoral Policy and Action: Recognizing that health is influenced by factors beyond the healthcare system (e.g., education, housing, environment), PHC promotes collaboration across sectors. This ensures policies in diverse areas contribute to better public health outcomes.
-
Empowering Individuals and Communities: This component focuses on equipping individuals, families, and communities to take charge of their health. This includes providing health education, promoting healthy lifestyles, and fostering community participation in health decision-making.
Rooted in social justice, equity, solidarity, and participation, PHC represents a transformative approach to healthcare, emphasizing accessibility, affordability, and community ownership.
Key Principles and Historical Context
The principles of WHO PHC are rooted in two landmark declarations:
-
The Alma-Ata Declaration (1978): This declaration marked a pivotal moment, highlighting health as a fundamental human right. It emphasized community involvement and intersectoral collaboration as essential for achieving “health for all.”
-
The Astana Declaration (2018): Reaffirming the Alma-Ata Declaration, the Astana Declaration underscored PHC as the foundation for UHC. It provides a renewed commitment to PHC, adapting its principles to the 21st century and outlining a roadmap for achieving UHC by 2030.
The Astana Declaration further defines PHC through three key pillars:
-
Empowered People and Communities: Individuals and communities are at the heart of PHC, actively participating in health management decisions.
-
Integrated Health Services: Providing seamless and comprehensive care throughout life, connecting preventive, curative, rehabilitative, and palliative services.
-
Multi-sectoral Policies: Addressing the wider determinants of health by integrating policies across various sectors, including education, housing, and environment.
These principles and historical declarations guide the implementation and future direction of WHO PHC, emphasizing its crucial role in promoting global health.
Implementing PHC: A Practical Roadmap
Translating principles into action requires a strategic approach. Implementing WHO PHC involves a multi-step process, tailored to specific community needs:
-
Assess Community Needs and Resources: Understand the unique health challenges, existing resources, and cultural context of the community. This involves gathering data, conducting surveys, and engaging with community members.
-
Develop a Tailored PHC Plan: Create a specific plan outlining goals, strategies, and activities, based on the community assessment. The plan may address specific health issues, target vulnerable populations, or strengthen existing health services.
-
Secure Necessary Resources: Mobilize resources, including funding, infrastructure, trained personnel (doctors, nurses, community health workers), essential medicines, and technologies.
-
Implement and Monitor: Put the plan into action and regularly monitor its progress. Track key indicators, evaluate outcomes, and adapt strategies as needed. Community feedback and participation are essential during this stage.
-
Engage Communities: Empower individuals and communities to actively participate in all stages of PHC implementation, from planning to evaluation. This ensures the program remains relevant, responsive, and sustainable.
-
Strengthen the Health System: PHC should not function in isolation but rather strengthen the entire health system. Improve referral mechanisms, integrate traditional medicine where appropriate, and invest in health workforce development.
The WHO offers resources and guidance to support countries in implementing PHC, including the publication “Implementing the Primary Health Care Approach: A Primer.” This guide offers detailed information and practical examples.
Benefits of PHC: Achieving Health for All
Investing in PHC yields significant benefits, impacting individuals, communities, and health systems globally:
- Improved Health Outcomes: PHC probably contributes to decreased maternal and child mortality rates, increased life expectancy, and reduced burden of infectious and chronic diseases.
- Reduced Health Inequities: By reaching vulnerable populations, PHC promotes health equity, ensuring everyone has a fair chance at a healthy life.
- Stronger Health Systems: PHC builds resilient health systems, better equipped to handle crises like disease outbreaks and natural disasters.
- Economic Benefits: Healthier populations likely lead to greater productivity and economic growth. Some experts believe PHC may offer a cost-effective approach to healthcare delivery in the long term.
The Future of PHC: Adapting to a Changing World
As the global health landscape evolves, PHC continues to adapt. Emerging challenges and opportunities include:
- Climate Change: Understanding and addressing the health impacts of climate change, integrating climate resilience into PHC strategies.
- Technological Advancements: Leveraging technology to improve access to care, particularly in remote areas, and enhance health information systems.
- Mental Health Integration: Recognizing the importance of mental health, integrating mental health services into PHC platforms.
Ongoing research and innovation are essential to further strengthen PHC. Exploring new service delivery models, evaluating program effectiveness, and adapting to evolving community needs will ensure PHC remains a powerful force in achieving health for all.
Disclaimer: This information is derived from publicly available content from the WHO and is intended for educational purposes. It is not a substitute for professional medical advice. For specific health concerns, consult with a healthcare professional.
- Sectioned Tupperware for Organized Meals and Snacks on the Go - March 7, 2026
- Meal Containers with Dividers Keep Foods Separate and Fresh - March 6, 2026
- Tupperware with Dividers Makes Entertaining Easy and Organized - March 5, 2026