Defining Minority Health and Health Disparities
This article clarifies the distinction between “minority health” and “health disparities,” two crucial concepts for understanding and addressing health inequities. These terms, while related, represent distinct perspectives on the health challenges faced by diverse populations.
Official Definitions
The National Institute on Minority Health and Health Disparities (NIMHD) provides the following definitions:
“Minority health” refers to the morbidity and mortality of American Indian/Alaska Native, Asian American, Black/African American, Hispanic/Latino, and Native Hawaiian/Other Pacific Islander populations in the United States. “Health disparities” are preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations. These populations are frequently defined by race/ethnicity, gender, socioeconomic status, age, disability, or sexual orientation. (NIMHD Website)
Key Differences: A Quick Reference
| Feature | Minority Health | Health Disparities |
|---|---|---|
| Focus | Health of specific racial/ethnic groups | Differences in health outcomes between groups |
| Scope | Examines health within a specific group | Compares health outcomes across groups |
| Goal | Understand and improve health within the group | Identify and reduce health outcome gaps |
Detailed Explanations
Minority Health: A Closer Look
Minority health examines the health status of racial and ethnic groups designated as minorities within a specific context, such as the United States. This involves investigating health issues prevalent in these groups, their access to healthcare, and the quality of care they receive. Factors such as cultural practices, geographic location, socioeconomic status, and experiences with discrimination can all significantly influence health outcomes within these populations.
Health Disparities: Unpacking the Inequalities
Health disparities represent differences in health outcomes between groups, often stemming from systemic disadvantages. These disparities are not simply variations in health; they are preventable gaps linked to social, economic, and environmental factors. These may include differences in access to resources like healthy food, safe housing, quality education, and healthcare. Crucially, health disparities can affect any group facing disadvantage, not just racial or ethnic minorities.
The Interplay of Minority Health and Health Disparities
Research in minority health frequently reveals health disparities. By closely examining the health profile of a specific minority group, researchers can identify areas where they experience worse health outcomes compared to other populations. Understanding the unique health context of a group allows for targeted interventions and policies aimed at reducing disparities.
Affected Populations
Officially Designated Minorities (OMB Directive 15):
- American Indian or Alaska Native
- Asian American
- Black or African American
- Native Hawaiian or Other Pacific Islander
- Hispanic or Latino
Populations Experiencing Health Disparities (NIH):
While the above list represents officially designated minorities, health disparities can impact various groups, including:
- Racial and ethnic minorities
- People with disabilities
- Individuals identifying as LGBTQ+
- People living in rural or underserved areas
- Individuals experiencing poverty or low socioeconomic status
- Other groups facing systemic disadvantage
Illustrative Examples of Health Disparities
Location Context
Health disparities often vary geographically. For instance:
- Diabetes: Higher rates of type 2 diabetes are observed in some Hispanic/Latino communities in the Southwestern United States, potentially influenced by factors like diet, genetics, and access to healthcare.
- Maternal Mortality: Black women in the Southern United States experience disproportionately high rates of maternal mortality compared to their White counterparts, highlighting the intersection of race and geography in shaping health outcomes.
- Rural Health: Individuals living in rural Appalachia may face disparities in access to specialized cancer care compared to those in urban areas with more healthcare resources.
Additional Examples
- Cardiovascular Disease: Black Americans have a higher prevalence of hypertension and heart disease compared to White Americans, likely influenced by social determinants of health and systemic factors.
- Cancer: Certain Asian American subgroups may experience higher rates of specific cancers, highlighting the diversity of health outcomes within the broader Asian American population.
- HIV/AIDS: Men who have sex with men, regardless of race/ethnicity, continue to be disproportionately affected by HIV/AIDS.
Related Concepts
- Health Equity: The attainment of the highest level of health for all people. This requires valuing everyone equally while addressing avoidable inequalities, historical and contemporary injustices, and the elimination of health and healthcare disparities.
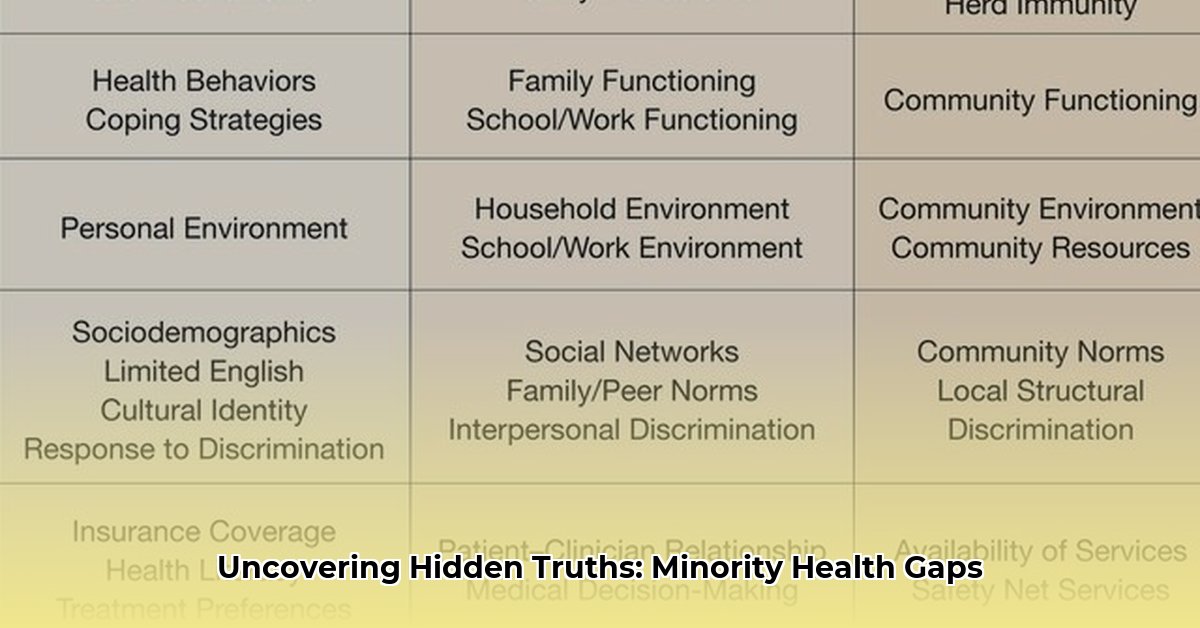
- Social Determinants of Health: The conditions in which people are born, grow, live, work, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. These include economic stability, education, social and community context, health and health care, and neighborhood and built environment.
- Healthcare Access: The timely use of personal health services to achieve the best health outcomes. This includes insurance coverage, availability of services, transportation, and cultural competency within the healthcare system.
Addressing Health Disparities
Efforts to address health disparities require a multi-pronged approach, including:
- Policy Changes: Implementing policies that promote health equity, such as expanding access to affordable healthcare, addressing systemic racism, and investing in underserved communities.
- Community-Based Programs: Developing and supporting programs tailored to the specific needs of communities experiencing disparities, focusing on prevention, education, and access to resources.
- Research: Continuing research to better understand the complex factors contributing to health disparities and develop more effective interventions.
- Culturally Competent Healthcare: Training healthcare providers to deliver culturally sensitive care and address implicit biases that may contribute to unequal treatment.
Conclusion
Understanding the distinctions between minority health and health disparities is paramount for advancing health equity. While minority health focuses on the health of specific groups, health disparities highlight the unequal outcomes resulting from systemic disadvantages. Addressing these disparities requires a continuous commitment to dismantling barriers to health and ensuring that everyone has a fair and just opportunity to achieve their highest level of health and well-being.
- Borosilicate Glass Containers Offer Superior Food Storage and Meal Prep - January 20, 2026
- Glass Lid Storage Containers Keep Food Fresh and Safe - January 19, 2026
- Borosilicate Glass Storage Delivers Durability and Safety for Meals - January 18, 2026