Nursing is more than just treating illnesses; it’s about caring for the whole person. Maslow’s Hierarchy of Needs provides a powerful framework for understanding and addressing the full spectrum of patient needs, from basic survival to emotional well-being. This guide explores how nurses can apply this framework to improve patient outcomes, enhance the nurse-patient relationship, and prepare for NCLEX success.
Understanding Maslow’s Hierarchy
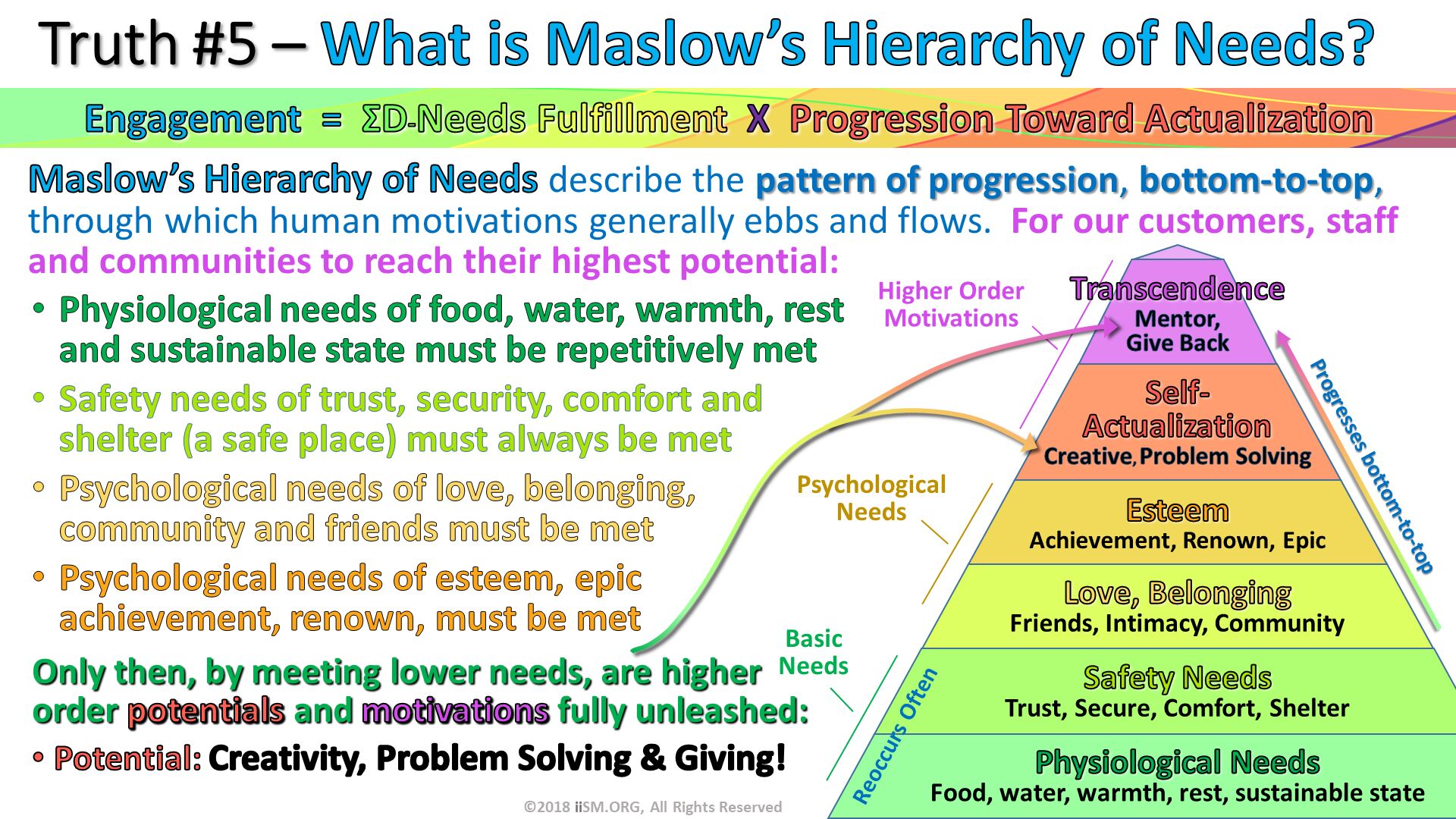
Maslow’s Hierarchy of Needs is a five-tier model of human motivation, often depicted as a pyramid. Developed by psychologist Abraham Maslow, it suggests that individuals are motivated to fulfill basic needs before progressing to more advanced ones. Let’s explore each level:
Physiological Needs: The Foundation of Life
These are the absolute essentials for survival: oxygen, water, food, shelter, sleep, thermoregulation, and elimination. In nursing, this translates to ensuring adequate oxygenation, providing proper nutrition and hydration, managing pain, and fostering a comfortable environment. Imagine trying to focus on anything else when you’re in pain or struggling to breathe!
Safety and Security Needs: Building Trust and Stability
Once physiological needs are met, the need for safety and security emerges. This includes physical safety (protection from harm and infection), as well as emotional security (feeling safe, stable, and trusting). Nurses address these needs by fostering a secure environment, providing clear and honest communication, and establishing predictable routines. Think about how important it is for a patient to feel safe in their surroundings and trust their healthcare team.
Love and Belonging Needs: Fostering Connection and Support
Humans are social creatures who crave connection, love, affection, and a sense of belonging. In nursing, this means facilitating communication with family and friends, providing emotional support, and fostering a sense of community. A simple act of kindness or a listening ear can profoundly impact a patient’s well-being.
Esteem Needs: Nurturing Self-Worth and Confidence
As patients feel more secure and connected, the need for self-respect, confidence, and achievement takes center stage. Nurses can bolster patients’ self-esteem by respecting their autonomy, promoting independence, and acknowledging their achievements. Celebrating even small victories can empower patients and foster resilience.
Self-Actualization Needs: Supporting Growth and Purpose
At the peak of the pyramid is self-actualization: the desire to reach one’s full potential and live authentically. This might involve pursuing creative outlets, finding meaning in experiences, or connecting with spirituality. While not always directly addressed in acute care settings, nurses can still support patients’ journeys toward self-actualization by encouraging goal setting and providing resources for personal growth.
Applying Maslow’s Hierarchy in Nursing Practice
Maslow’s Hierarchy isn’t simply a theory; it’s a practical guide for providing patient-centered care. Here’s how it translates to real-world nursing:
Prioritizing Patient Care
Maslow’s framework guides nurses in prioritizing interventions. Physiological needs (e.g., airway, breathing, circulation) take precedence over psychosocial needs. A patient experiencing respiratory distress, for instance, requires immediate attention to their oxygen needs before addressing emotional concerns. This prioritization is a critical skill for NCLEX success.
Holistic Patient Assessment
The hierarchy encourages a comprehensive assessment that considers all levels of needs, ensuring no crucial area is overlooked. This helps nurses gain a deeper understanding of each patient’s unique circumstances and develop individualized care plans.
Individualized Care Planning
Recognizing that every patient is unique, Maslow’s framework helps tailor interventions to meet individual needs. For example, a patient recovering from surgery may initially focus on pain management (physiological), while later prioritizing emotional support and a sense of normalcy (love and belonging, esteem).
Examples in Nursing Specialties
- Medical-Surgical: Managing post-operative pain (physiological), preventing falls (safety), addressing anxiety about diagnosis (safety/security).
- Critical Care: Ensuring adequate ventilation (physiological), preventing infections (safety), providing emotional support to families (love/belonging).
- Pediatrics: Providing age-appropriate nutrition (physiological), creating a safe play environment (safety), supporting parent-child bonding (love/belonging).
- Mental Health: Establishing a therapeutic relationship (safety/security, love/belonging), promoting self-care activities (esteem), supporting recovery goals (self-actualization).
Maslow’s Hierarchy in Challenging Situations
Complex Patients
Patients with multiple health conditions often have overlapping needs. Maslow’s framework helps nurses navigate these complexities. For example, a patient with chronic pain (physiological) might also experience isolation and depression (love/belonging). Addressing both physical and psychosocial needs is crucial for improving overall well-being.
Ethical Dilemmas
The hierarchy can inform ethical decision-making in challenging situations. For example, when resources are limited, nurses may need to prioritize patients with the most urgent physiological needs.
Global Pandemic Context and Nurse Well-Being
The COVID-19 pandemic highlighted the critical importance of addressing healthcare workers’ needs. When nurses’ own safety, security, and emotional well-being are compromised, their ability to provide effective patient care is also impacted. Applying Maslow’s hierarchy to support nurses themselves is equally vital for a healthy healthcare system.
Beyond the Pyramid: Expanding Maslow’s Framework
While Maslow’s Hierarchy offers valuable insights, it’s essential to acknowledge its limitations. The rigid structure may not always reflect the fluidity of human experience, and cultural factors can influence how needs are prioritized. Ongoing research continues to explore these nuances.
Criticisms and Adaptations
Some critics argue that the hierarchy is too simplistic and doesn’t account for individual differences or cultural variations. Adapting the framework to consider these factors is vital for providing culturally sensitive care. For instance, some cultures prioritize community over individual achievement, influencing how self-actualization is perceived and pursued.
Newer Interpretations: Transcendence
Some researchers suggest adding a level beyond self-actualization: transcendence. This level represents a focus on something beyond the self, such as spirituality, altruism, or contributing to a greater cause. While still under investigation, this concept expands the framework and acknowledges the diverse range of human motivations.
Conclusion
Maslow’s Hierarchy of Needs is a valuable framework for understanding and meeting patient needs. By using this framework thoughtfully and recognizing its limitations, nurses can provide compassionate, holistic care that truly makes a difference. This patient-centered approach leads to better outcomes, strengthens the nurse-patient relationship, enhances patient satisfaction, and improves the efficiency of nursing time.
Memory loss can significantly impact an individual and their relationships. Discover the impact of memory loss strain. Neurofeedback has shown promise in treating certain conditions, but some claim negative experiences. Explore neurofeedback ruined my life for a different perspective.
- Separated Lunch Containers Keep Different Foods Fresh and Organized - February 13, 2026
- Divided Containers Simplify Meal Prep for Busy Individuals - February 12, 2026
- Why Sectioned Food Containers Are Best for Meal Prep - February 11, 2026