Losing a tooth can have a major impact, but fortunately, restoring your smile and jawbone health is possible. This guide explains bone grafting, a procedure often performed following tooth extraction, covering the types of bone grafts available, their costs, and effectiveness. For more information on bone graft costs, see this helpful resource: Bone Graft Costs. We provide a comprehensive overview, including expert insights, potential issues, and preventative and post-operative care measures for achieving the best outcomes. This informational article aims to provide patients and dental professionals with actionable intelligence on bone grafting.
Understanding Bone Loss and the Importance of Bone Grafting After Extraction
Following a tooth extraction, the jawbone can weaken and lose density over time, similar to how a house loses stability when a support beam is removed. This occurs because the jawbone relies on the tooth’s root for stimulation. Extraction with a bone graft helps rebuild the jawbone, prevents future complications, and sets the stage for a healthier smile. Bone grafting is a preventative measure against bone loss, crucial for maintaining the jaw’s structural integrity and aesthetic appearance. Without the tooth’s root stimulating the bone, the alveolar bone (the part of the jawbone that surrounds and supports the teeth) begins to resorb, or break down. This resorption can lead to a decrease in bone volume, both in width and height.
The Benefits of Extraction with Bone Grafting: Why Choose This Procedure?
Choosing extraction with bone grafting offers several advantages. It helps maintain the structural integrity of your jaw, making it a proactive measure against future bone loss. Secondly, it prepares the area for dental implants by ensuring enough healthy jawbone is available to stably support them. Finally, it improves the aesthetics of your teeth by keeping the jawbone’s structure intact, avoiding the sunken look that can occur after an extraction. A bone graft also supports the surrounding teeth and prevents shifting or instability that can occur when bone loss weakens the foundation. Considering these benefits, is a bone graft the right choice for preserving your jaw’s health and appearance?
- Prevents further bone loss, maintaining structural integrity and preventing a sunken facial appearance.
- Sets the stage for successful dental implant placement, providing a stable base.
- Improves smile aesthetics by preserving the natural jawline and supporting surrounding teeth.
- Reduces the risk of future dental problems related to bone loss, such as adjacent tooth instability.
Exploring the Types of Bone Grafts: Which Option is Right for You?
There are various types of bone grafts, each offering different advantages and disadvantages. Your dentist will help determine the best choice for your needs. Understanding these options is essential for making informed decisions about your dental health.
| Graft Type | Source | Advantages | Disadvantages |
|---|---|---|---|
| Autograft | Your own body | Best chance of integrating, lowest risk of rejection, contains live bone cells | Requires a second surgical site for bone harvesting; slightly more painful; limited bone availability |
| Allograft | Donor bone (deceased) | Readily available, avoids a second surgical site | Minor risk of disease transmission (though extremely rare due to stringent screening), potential for slower integration |
| Xenograft | Animal bone (e.g., cow, pig) | Biocompatible, commonly available, good structural support | Higher risk of rejection compared to autografts, ethical concerns for some patients |
| Alloplast | Synthetic bone substitute (calcium phosphate, hydroxyapatite) | No risk of disease transmission, readily available, unlimited supply | May not integrate as well as natural bone, can be brittle; possibility of long-term issues |
The right choice depends on factors like bone loss extent, overall health, cost considerations, and patient preferences. The size and location of the defect also play a role in determining the graft type.
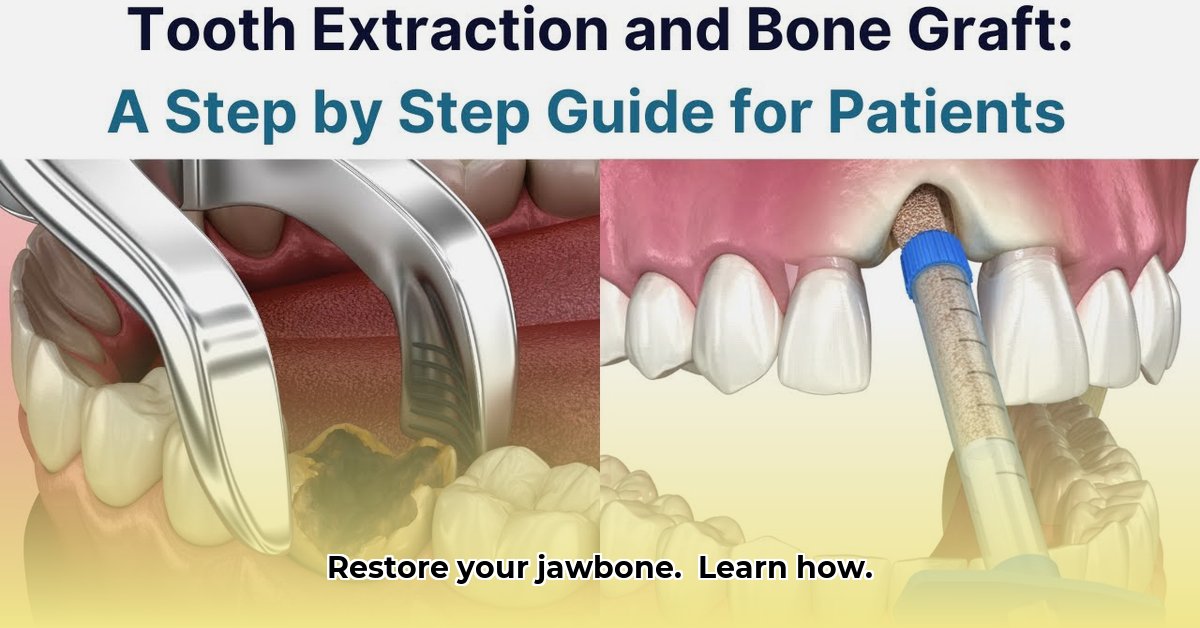
Step-by-Step Guide to the Extraction with Bone Graft Procedure
The procedure typically involves these steps: tooth extraction, site preparation, bone graft placement, and site closure. The total time can vary from 30 minutes to several hours, depending on the complexity of the extraction and the type of bone graft used. Some procedures can be completed in under an hour, while more complex cases, such as those involving significant bone loss or the need for a membrane, may take longer.
- Tooth Extraction: The dentist carefully and atraumatically removes the problematic tooth, minimizing trauma to the surrounding bone.
- Site Preparation: The extraction site is thoroughly cleaned of any debris or infected tissue and prepared for the bone graft. This may involve shaping the socket to optimize graft placement.
- Bone Graft Placement: The chosen bone graft material is carefully placed into the socket, filling the void left by the extracted tooth. The material is often packed tightly to ensure stability.
- Membrane Placement (Optional): In some cases, a collagen membrane is placed over the bone graft to protect it and prevent soft tissue from growing into the graft site. This membrane promotes bone regeneration.
- Site Closure: The area is closed using stitches, which help to stabilize the graft and promote healing. The stitches are typically removed after 1-2 weeks.
Post-Operative Care: Ensuring Successful Jawbone Healing
Following your dentist’s instructions is essential for successful healing after a bone graft. Instructions include taking prescribed pain medication, following a soft food diet, avoiding strenuous activities and maintaining oral hygiene. Proper post-operative care is crucial for preventing infection, promoting bone regeneration, and ensuring the long-term success of the graft.
- Take pain medication as directed to manage discomfort and reduce inflammation.
- Follow a soft food diet to avoid putting pressure on the graft site.
- Avoid strenuous activities that could disrupt the healing process.
- Maintain meticulous oral hygiene, gently cleaning the area around the graft site.
- Use an antibacterial mouthwash as prescribed by your dentist.
- Avoid smoking, as it can impair healing and increase the risk of complications.
- Attend all scheduled follow-up appointments to monitor healing and address any concerns.
Adhering to post-operative instructions minimizes complications and ensures graft integration. Failure to follow instructions can lead to infection, graft failure, and the need for additional procedures.
Understanding Potential Risks and Complications
While generally safe, extraction with a bone graft carries potential risks, including infection, swelling, pain, nerve damage, and graft rejection. These risks are uncommon with proper care and adherence to post-operative instructions. It is also possible to experience sinus complications if the graft is in the upper jaw near the sinus cavity.
“It is important to discuss potential complications with your dentist before the procedure to make an informed decision,” said [Dr. Michael Brown], [Board Certified Oral and Maxillofacial Surgeon] at [Coastal Oral Surgery]. “Understanding the risks and benefits allows patients to actively participate in their treatment plan.”
Determining If Extraction with Bone Grafting Is Right for You
The decision to get a bone graft during or after extraction depends on bone loss, oral health, and future dental plans. A dentist consultation is crucial to determine if it’s the right choice. Factors such as the location of the extracted tooth, the condition of the surrounding bone, and whether or not you plan to get a dental implant will influence the recommendation. In some cases, bone grafting may not be necessary if the bone loss is minimal and a dental implant is not planned. However, in most cases, a bone graft is highly recommended to preserve bone volume and ensure the possibility of future implant placement.
Choosing the Best Bone Graft Material for Dental Implants: A Comprehensive Guide
Successful dental implants often require bone grafting to ensure sufficient jawbone density. Choosing the right bone graft material is a critical decision that can significantly impact the success of your dental implant procedure. The selection hinges on various factors, including the extent of bone loss, bone quality, patient health, and surgical site accessibility. The best option depends on individual circumstances and the specific needs of your case. Some materials are better suited for smaller defects, while others are designed for larger reconstructions.
Understanding Bone Graft Material Options
Understanding your options when learning how to choose the best bone graft material for dental implants, is like choosing the right materials to build a house’s foundation to guarantee stability and longevity. Bone graft materials commonly used include autografts (bone from your own body, thought to be the “gold standard”), allografts (bone from a deceased donor), xenografts (animal-derived bone), and alloplasts (synthetic). Autografts are naturally compatible and promote excellent bone regeneration, while allografts are readily available and less invasive. Xenografts are biocompatible and commonly available, while alloplasts are synthetic and carry no risk of disease transmission. However, each has different characteristics. Which material suits your needs best? The ideal material should be biocompatible, promote bone regeneration, and be easy to handle during surgery.
- Autografts: Your own bone, offering excellent compatibility and the highest success rate.
- Allografts: Donor bone, readily available but with a slight risk of immune reaction or delayed healing.
- Xenografts: Animal bone, less expensive but potentially lower success rates and ethical considerations.
- Alloplasts: Synthetic, which carry no risk of disease transmission and offer predictable results.
Factors Influencing Material Selection: The Decision-Making Process
Your oral surgeon will examine numerous factors, including the extent of bone loss, bone quality, and patient health, and surgical site accessibility. These factors guide the selection of the most suitable graft material. The surgeon will also consider your medical history, any allergies you
- Rectangular Glass Food Storage Containers For Meal Prep - January 27, 2026
- Borosilicate Glass Food Containers Keep Meals Fresh and Organized - January 26, 2026
- Choosing Glass Containers With Snap Lids for Fresh Food Storage - January 25, 2026