Do your zip code, income, or even your appearance seem to dictate your health? In America, this is often a stark reality. This isn’t about luck; it’s about deeply entrenched systems creating barriers to health for some, while others thrive. This article investigates why these health disparities exist, exploring how power imbalances and unequal access to resources like healthcare and nutritious food create a system where some flourish, and others struggle. We’ll examine the roles of racism, sexism, and classism, and how even unconscious biases in healthcare settings can worsen these disparities. Our goal isn’t just to identify the problems but to dissect the systemic issues at their core and explore potential solutions.
Unequal Health: Unpacking the “Why”
What are health disparities? Imagine two neighboring towns. One boasts pristine parks, grocery stores brimming with fresh produce, and well-funded schools. The other grapples with pollution, fast-food outlets on every corner, and struggling schools. It’s likely the second town’s residents face greater health challenges. Health disparities are these differences in health outcomes—life expectancy, disease prevalence—linked to factors like location, race, income, disability, sexual orientation, and gender identity. These differences aren’t random; they’re often the product of unfair systems and practices.
A core issue is power. Who determines resource allocation? Who decides where parks are built or which neighborhoods receive better healthcare access? Often, those already possessing ample resources make these decisions, sometimes unintentionally (and sometimes intentionally) leaving others behind. This uneven distribution of resources—good schools, safe housing, healthy food—fuels health disparities. Chronic stress from financial insecurity or living in a high-crime area makes focusing on health incredibly difficult.
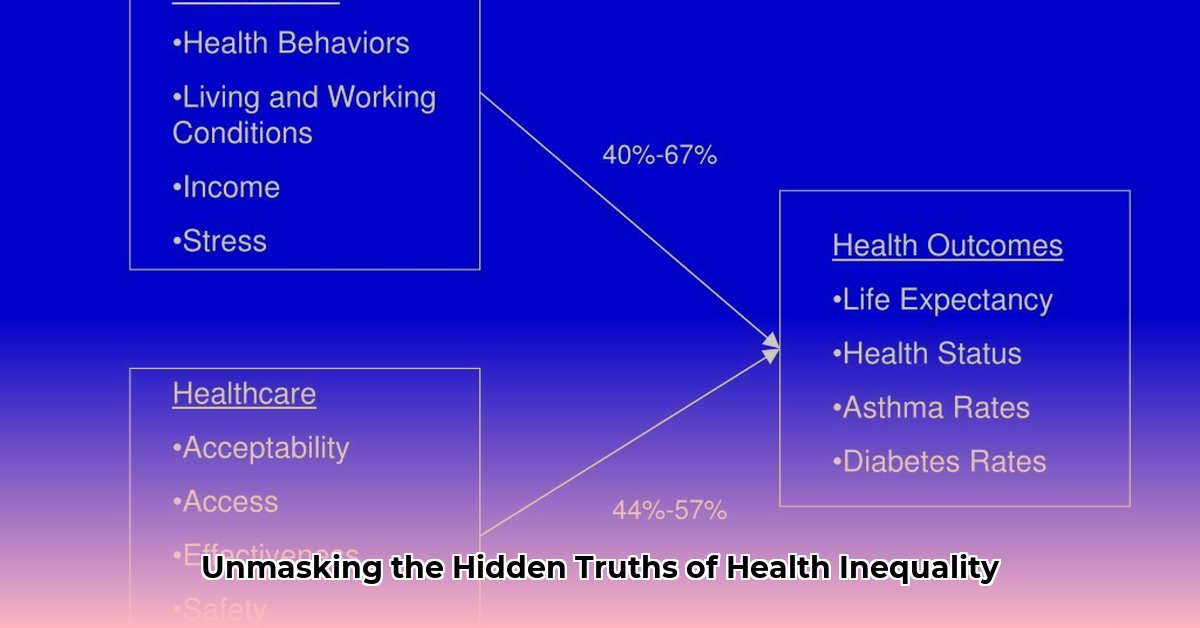
Social determinants of health—the conditions in which we live, work, and age—play a significant role. Consider healthcare access. Even with insurance, reaching a distant clinic without a car can be a major obstacle. Long working hours for low wages may preclude preventative care. Living in a “food desert” limits access to fresh produce while processed foods abound. These intertwined social determinants profoundly influence our health.
Even when individuals from diverse backgrounds access healthcare, quality of care can vary significantly. Implicit bias—unconscious prejudice—can infiltrate healthcare settings. Well-intentioned doctors and nurses may unknowingly treat patients differently based on race, ethnicity, or other characteristics. Studies suggest pain medication might be prescribed less frequently to people of color, possibly reflecting biases about pain tolerance. These biases contribute to unequal outcomes. For instance, maternal mortality rates are significantly higher for Black women than white women, likely due in part to implicit bias within the healthcare system.
Disparities Decoded: Exposing the Root Causes
Why do these disparities persist? Systemic inequalities—deep-seated disadvantages woven into our societal fabric—create an uneven playing field.
Racism, for example, isn’t just individual prejudice; it’s a system woven into institutions and policies, creating health barriers for certain groups. This manifests in unequal access to quality healthcare, jobs with health insurance, nutritious food, and safe housing. Sexism, classism, homophobia, xenophobia, and ableism also contribute to this uneven distribution of well-being, hindering certain communities from reaching their full health potential.
Our environment—our neighborhoods and communities—are also critical. Social determinants of health profoundly influence our well-being. Growing up in a neighborhood lacking a grocery store with fresh produce or facing high crime rates and limited park access significantly impacts health outcomes. Access to healthy food, quality education, safe housing, reliable transportation, and clean air shape our choices and opportunities, affecting everything from stress levels to chronic disease risk.
Economic stability is another key factor. Financial strain, unemployment, and unstable housing create constant stress, hindering healthy choices and access to quality medical care. Education empowers individuals to understand health information and navigate the healthcare system. Lack of quality education creates yet another hurdle. Access to affordable healthcare, including insurance and culturally competent doctors, is essential. Limited access widens the health gap between the privileged and the marginalized.
Intersectionality further complicates the picture. Different forms of discrimination intersect and overlap, creating unique challenges. A woman of color faces challenges related to both her race and gender, impacting her access to quality healthcare. A person with a disability from a low-income background encounters obstacles due to ableism and classism. These intersecting identities compound existing health disparities.
Table: Root Causes of Health Disparities
| Cause | Description | Example |
|---|---|---|
| Structural Racism | Systemic disadvantages based on race embedded within societal structures and institutions. | Residential segregation limiting access to healthy food options and quality healthcare. |
| Sexism | Discrimination based on gender, leading to unequal opportunities and outcomes. | Unequal pay for women, impacting their ability to afford healthcare. |
| Classism | Discrimination based on socioeconomic status, creating barriers to resources and opportunities. | Lack of access to quality education limiting job opportunities and income, affecting access to healthcare. |
| Social Determinants of Health | Conditions where people are born, live, learn, work, play, worship, and age that affect health. | Lack of healthcare access due to lack of insurance or transportation. |
This simplified overview highlights interconnected and complex challenges. Ongoing research adds to our understanding of these interactions. There’s no quick fix, but acknowledging the root causes is the first step toward building more equitable systems supporting everyone’s well-being.
Power Dynamics and Health: A Deeper Dive
How do systems of power—the often invisible forces—shape our well-being? These systems determine who accesses essential resources, opportunities, and even respect. This unequal distribution lies at the heart of health disparities.
1. Access: The Foundation of Health: Power shapes access to basic needs like housing, food, education, and employment. When people lack power, these essentials become harder to attain. This power imbalance creates unequal health outcomes from the outset.
2. Discrimination: A Barrier to Well-being: Power imbalances fuel prejudice and discrimination. Implicit biases in healthcare can lead to unequal treatment. Microaggressions—subtle acts of discrimination—erode self-worth and increase stress, taking a physical toll and increasing the risk of chronic conditions.
3. The Cycle of Disadvantage: Lack of political power hinders marginalized groups from advocating for change, perpetuating disadvantage and impacting mental and physical well-being.
4. Breaking the Cycle: Creating a healthier society requires dismantling discriminatory structures and rethinking resource distribution. This involves policies prioritizing social determinants of health, empowering communities, and providing them with resources to thrive.
Perspectives on Health Equity: Achieving health equity has no easy answer. Some focus on systemic reforms, others on community interventions, and still others on policy changes addressing broader inequalities. A combination of strategies is likely needed.
Limits of Current Knowledge: Our understanding of how power dynamics influence health continues to evolve. Ongoing research explores the interplay of social, economic, environmental, and cultural influences. While evidence links power imbalances to health disparities, much remains unknown. Further research is crucial for developing more effective strategies for health equity.
Table: Power Dynamics and Health Impacts
| Aspect of Power Dynamics | Potential Health Impacts |
|---|---|
| Limited healthcare access | Increased preventable illnesses, poorer disease management |
| Environmental hazards | Elevated risk of respiratory problems, cancer |
| Discrimination stress | Higher rates of cardiovascular disease, mental health issues |
| Lack of healthy food | Increased risk of obesity, diabetes |
| Inadequate housing | Increased risk of infections, respiratory illnesses |
This table simplifies complex and nuanced relationships. The influence of power dynamics can intersect, creating layers of disadvantage. While we’ve made progress, much remains to be learned.
Unequal Resources, Unequal Health: A Closer Look
How does uneven resource distribution impact health? It’s not just about lack of access; it’s about the ripple effects across entire communities. Unequal distribution of healthcare resources (hospitals, clinics, equipment, qualified professionals) creates a divide between the “haves” and “have-nots” in healthcare, impacting health outcomes and potentially leading to preventable illnesses and premature deaths.
Unequal resource allocation is intertwined with other social determinants of health—poverty, education, housing. Poverty may limit access to nutritious food, contributing to poor health. Substandard housing exposes residents to environmental hazards. These interwoven factors create a challenging cycle to break.
Historical context is also crucial. Past policies like redlining have lasting effects on communities, creating disparities in healthcare, education, and economic opportunities. Understanding this context informs strategies for addressing the root causes of unequal resource allocation. Investments in community health centers and programs addressing social determinants can mitigate the impact of historical injustices.
Socioeconomic factors—poverty, lack of education, unemployment—contribute significantly to poor health. Constant financial worry hinders prioritizing doctor’s appointments and healthy eating, leading to preventable illnesses becoming serious due to lack of early intervention.
Race, ethnicity, and location also play significant roles. Certain racial and ethnic groups are concentrated in areas with fewer resources. Combining this with socioeconomic factors creates significant health disparities. Living in a rural area far from specialists or hospitals makes getting needed care incredibly difficult.
Implicit bias—unconscious biases healthcare providers might have—can lead to different treatment, misdiagnoses, and lack of trust between patients and doctors. These biases impact health journeys.
Addressing this requires a multifaceted approach:
- Policy Changes: Invest in underserved communities, ensuring equal access to healthcare facilities, technology, and qualified professionals.
- Community Interventions: Utilize community health workers who understand local needs, bridge cultural and linguistic gaps, build trust, and increase healthcare accessibility.
- Addressing Implicit Bias: Provide training and education to healthcare providers to promote awareness of biases and develop strategies for equitable care.
Table: Factors Impacting Resource Allocation and Health
| Factor | Potential Impact |
|---|---|
| Socioeconomic Status | Limited healthcare access, poorer outcomes due to cost concerns |
| Race/Ethnicity | Disparities in quality healthcare access, higher chronic illness rates, potential bias in healthcare |
| Geographic Location | Limited access to facilities and specialists, transportation challenges hindering timely care |
| Healthcare System Factors | Insurance coverage and provider availability influencing access to care |
Our understanding of these factors is constantly evolving. New research emerges, changing best practices. Addressing healthcare disparities isn’t just about fixing a system; it’s about investing in people and building healthier, more equitable communities where everyone can thrive.
- Separated Lunch Containers Keep Different Foods Fresh and Organized - February 13, 2026
- Divided Containers Simplify Meal Prep for Busy Individuals - February 12, 2026
- Why Sectioned Food Containers Are Best for Meal Prep - February 11, 2026