This guide provides NHS-backed advice on understanding and managing hiatus hernia symptoms through diet and lifestyle adjustments.
What is a Hiatus Hernia?
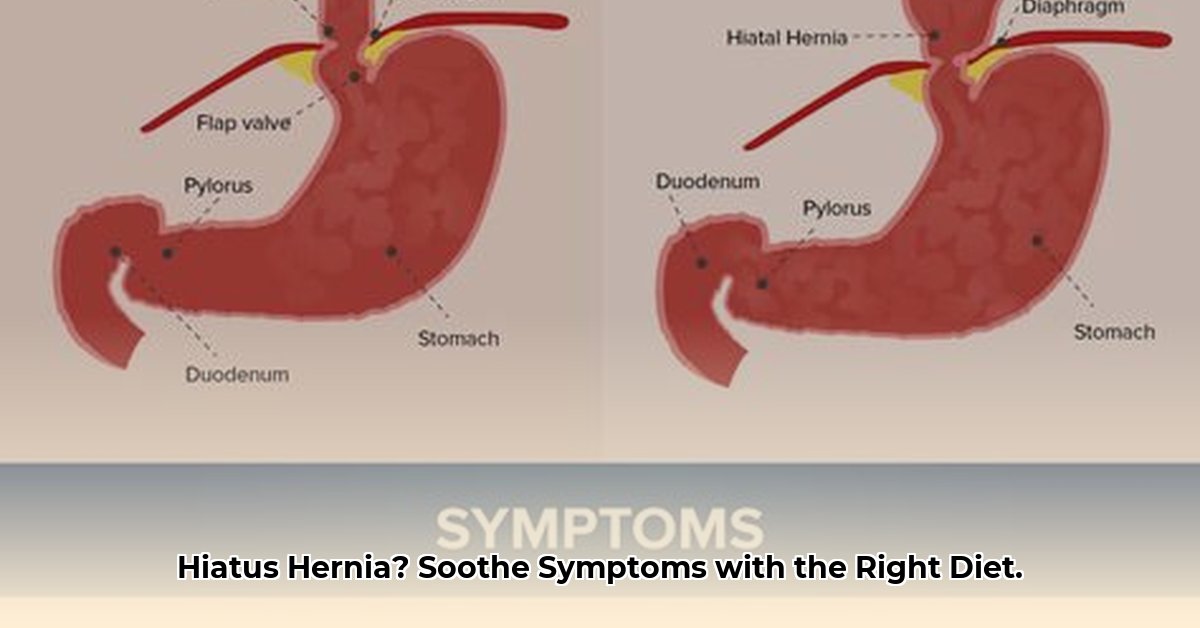
A hiatus hernia occurs when a portion of your stomach pushes upward through an opening in your diaphragm, called the hiatus. This hiatus normally allows your esophagus (food pipe) to pass through to your stomach. While many people with a hiatus hernia experience no symptoms, others may experience discomfort.
(Diagram of a normal diaphragm and one with a hiatus hernia would be placed here)
Recognizing the Symptoms
Hiatus hernias can cause a range of symptoms, primarily due to stomach acid refluxing into the esophagus. These may include:
- Heartburn: A burning sensation in the chest, often after eating, sometimes spreading to the throat.
- Acid reflux: A sour or bitter taste in your mouth caused by stomach acid coming back up.
- Regurgitation: Bringing up small amounts of food or bitter-tasting fluids.
- Difficulty swallowing (dysphagia): A feeling of food sticking in your throat or chest.
- Chest pain: Sometimes mistaken for heart pain, but typically related to acid reflux.
- Bloating and discomfort: Especially after meals.
- Nausea: A feeling of sickness.
- Bad breath (halitosis).
Some individuals experience no noticeable symptoms at all. If you’re concerned about any of these symptoms, always consult your GP.
Managing Your Hiatus Hernia: NHS Advice
Diet and lifestyle changes can significantly improve hiatus hernia symptoms. While the NHS doesn’t provide a strict list of prohibited foods, certain foods and habits are more likely to trigger symptoms. It’s important to identify your personal triggers and make adjustments accordingly.
Diet Management
Foods That May Trigger Symptoms:
- High-Fat Foods: These can relax the lower esophageal sphincter (LES), the valve between your esophagus and stomach, allowing acid reflux. Examples include fatty meats, fried foods, and rich sauces.
- Spicy Foods: These can irritate the esophagus, exacerbating existing discomfort.
- Acidic Foods: Citrus fruits, tomatoes, and tomato-based products can increase acidity and worsen heartburn.
- Onions and Garlic: These may relax the LES, similar to fatty foods.
- Chocolate, Caffeine, and Alcohol: These substances can also relax the LES and increase acid production.
- Carbonated Drinks: These can increase stomach pressure and worsen reflux.
- Peppermint: Though soothing for some digestive issues, peppermint can relax the LES.
Foods to Consider:
- Fiber-Rich Foods: Fruits (excluding citrus if it’s a trigger), vegetables, and whole grains promote healthy digestion.
- Lean Protein: Chicken, fish, beans, and lentils offer essential nutrients without the added fat of red meat.
- Probiotic-Rich Foods: Yogurt and kefir may contribute to a healthy gut environment, which could help with symptom management, although more research is needed.
- Non-Citrus Fruits: Apples, bananas, pears, and berries provide nutrition without the acidity of citrus fruits.
Lifestyle Changes
- Elevate Your Bed: Raise the head of your bed by 6-8 inches (15-20 cm) using bed risers or blocks. Do not use extra pillows, as this primarily elevates your head and not your chest. This helps gravity prevent acid reflux while sleeping.
- Smaller, More Frequent Meals: Eating smaller meals puts less pressure on your stomach and reduces the risk of reflux.
- Timing of Meals: Avoid eating anything for 2-3 hours before bedtime to allow your stomach to empty.
- Weight Management: If you’re overweight or obese, losing weight can significantly reduce pressure on your abdomen, easing symptoms.
- Quit Smoking: Smoking weakens the LES.
- Loose Clothing: Tight clothing can constrict the abdomen and worsen reflux.
- Stress Management: Stress can exacerbate digestive problems. Consider relaxation techniques like yoga or meditation.
When to Seek Medical Advice (NHS)
While lifestyle changes often help, consult your GP if:
- Symptoms persist or worsen despite self-care.
- You have difficulty swallowing or persistent vomiting.
- You experience unexplained weight loss.
- You see blood in your vomit or stools (poo).
Treatment Options (NHS)
The NHS offers various treatment options for hiatus hernia, ranging from lifestyle advice and over-the-counter medications (like antacids and alginates) to prescription medications and even surgery in severe or complicated cases. Your GP will determine the most suitable treatment plan for your individual circumstances.
Frequently Asked Questions (FAQ)
- Can a hiatus hernia be cured? In many cases, lifestyle changes and medical management can effectively control symptoms. Surgery can sometimes repair the hernia itself, but it’s not always necessary. Some research suggests a link between gut microbiome and symptom severity, but more studies are needed.
- Will I need surgery? Surgery is usually a last resort for severe cases or complications and is often a minimally invasive keyhole procedure.
Disclaimer
This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for diagnosis, treatment, and personalized recommendations.
NHS Resources
This comprehensive guide provides practical, NHS-approved advice on managing hiatus hernia symptoms through diet and lifestyle changes, empowering you to take control of your health and well-being. Remember, consulting your GP is crucial for personalized guidance and treatment.
- Food Prep Lunch Box Simplifies Healthy Meals for On-the-Go Lifestyles - February 18, 2026
- Choosing the Best Meal Prep Lunch Box for Daily Use - February 17, 2026
- Sectioned Food Storage Containers Are Your New Meal Prep Lifesaver - February 16, 2026