Access to quality primary healthcare is a cornerstone of a healthy society. Yet, for millions worldwide, this fundamental right remains elusive. This article delves into the complex web of challenges hindering primary healthcare, exploring the obstacles, their far-reaching consequences, and potential pathways towards a more equitable and sustainable future.
The Tangled Web: Key Challenges in Primary Healthcare
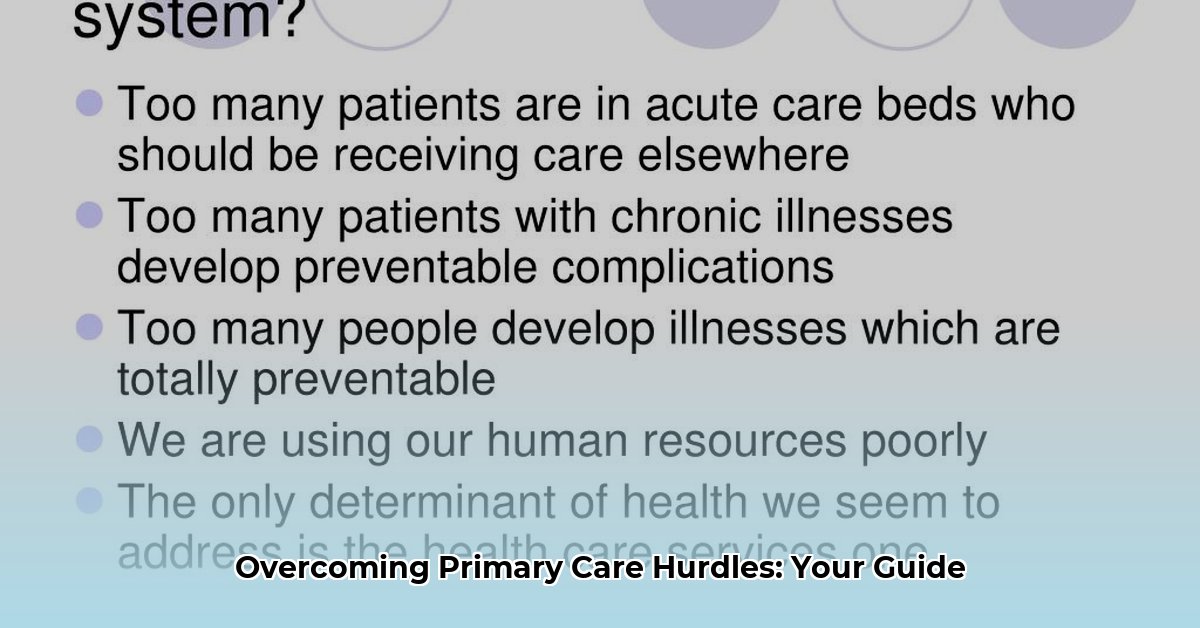
The challenges plaguing primary healthcare are multifaceted and interconnected, creating a complex system that demands comprehensive solutions.
Funding and Systemic Shortcomings
Chronic underfunding casts a long shadow over primary healthcare systems. Insufficient resources hamper the ability of clinics to invest in essential infrastructure, maintain up-to-date technology, and recruit and retain qualified staff. Inefficient administrative processes and poor coordination between different levels of care further exacerbate the strain on resources, leading to a fragmented and frustrating patient experience. These systemic issues create a ripple effect, impacting every aspect of primary care delivery.
The Workforce Strain: A Growing Crisis
A global shortage of healthcare professionals, including doctors, nurses, and community health workers, is a critical challenge. This scarcity is particularly acute in underserved areas, both rural and urban. The existing workforce often faces overwhelming workloads, leading to burnout and high turnover rates. Limited opportunities for training and professional development further compound the problem, hindering the ability of healthcare providers to stay abreast of the latest medical advancements.
Access Denied: Barriers to Entry
For many, accessing primary care is a formidable challenge. Geographic isolation, particularly in rural areas, creates significant barriers. Poverty and lack of insurance make healthcare unaffordable for a substantial portion of the population. Cultural and linguistic differences can impede effective communication between patients and providers. Discrimination based on race, ethnicity, gender, or sexual orientation further marginalizes vulnerable populations, creating additional hurdles to accessing essential care.
The Quality Quandary: Ensuring Effective Care
Even when access is secured, concerns about the quality of care often persist. Limited access to essential medications and diagnostic tools hinders effective treatment. Reliance on outdated practices, rather than evidence-based approaches, compromises patient outcomes. The pressure to address immediate health issues often overshadows the importance of preventative care, which is crucial for long-term well-being.
The Cost Conundrum: A Growing Burden
The escalating cost of healthcare services, including medications, diagnostic tests, and consultations, poses a significant financial burden on individuals and families. This often leads to delayed or forgone care, exacerbating health problems and ultimately increasing healthcare costs in the long run.
Shifting Demographics and Disease Burden: A Changing Landscape
An aging global population and the rising prevalence of chronic diseases, such as diabetes and heart disease, place unprecedented strain on primary healthcare systems. The emergence of new infectious diseases further complicates the landscape, requiring adaptable and resilient healthcare infrastructure.
The Engagement Enigma: Empowering Patients
Patient engagement – active participation in one’s own health – is essential for effective primary care. However, limited health literacy, mistrust in the healthcare system, and cultural beliefs can create a disconnect between patients and providers. Empowering patients to become informed and active participants in their care is crucial for improving health outcomes.
Charting a Course: Potential Solutions and Innovations
Addressing the complex challenges in primary healthcare requires a multi-pronged approach, incorporating innovative solutions and collaborative efforts.
| Primary Health Care Challenge | Potential Solutions |
|---|---|
| Funding and Systemic Issues | Increased and sustained funding, streamlined administrative processes, modernized infrastructure and technology, enhanced care coordination |
| Workforce Strain | Recruitment and retention initiatives, expanded training opportunities, improved working conditions, broadened scope of practice for nurses and other healthcare professionals |
| Access Barriers | Telehealth expansion, mobile clinics, transportation assistance, culturally competent care, addressing social determinants of health |
| Quality Concerns | Implementing evidence-based guidelines, quality improvement initiatives, increased access to essential medications and diagnostic tests, emphasis on preventative care |
| Escalating Costs | Cost containment strategies, wider use of generic medications, price transparency, preventative care to reduce long-term expenses |
| Shifting Demographics and Disease Burden | Chronic disease management programs, community health worker expansion, investment in geriatric care, strengthened public health initiatives |
| Patient Engagement Gap | Patient education programs, improved communication strategies, shared decision-making, culturally sensitive care, addressing health literacy |
Regional Variations: A Global Perspective
The specific challenges and effective solutions in primary healthcare vary significantly across different regions and countries, influenced by factors such as economic development, healthcare infrastructure, cultural norms, and government policies. Understanding these regional variations is crucial for developing tailored interventions.
The Future of Primary Care: A Call to Action
The future of primary healthcare hinges on our collective commitment to addressing these critical challenges. Ongoing research and innovation are essential for developing and implementing effective solutions. Collaboration between governments, healthcare providers, communities, and individuals is paramount. By working together, we can build a future where everyone has access to the quality primary care they deserve. This includes exploring the potential of artificial intelligence, investigating the role of social determinants of health, and carefully considering the ethical implications of technological advancements.
Why Primary Care Matters: A Foundation for Health
Primary care serves as the bedrock of a healthy life, providing a crucial link between individuals and the broader healthcare system. It emphasizes prevention, early detection, and chronic disease management, leading to improved health outcomes and reduced healthcare costs in the long run. By fostering strong patient-physician relationships, primary care empowers individuals to take an active role in their own well-being. However, access to this vital service remains unevenly distributed, with significant disparities based on factors like socioeconomic status, geographic location, and cultural background.
The Crisis in Primary Care: Addressing Workforce Shortages
The looming shortage of primary care physicians is a pressing concern. Factors contributing to this crisis include an aging physician population, high medical school debt, and the allure of higher-paying specialties. The consequences of this shortage are far-reaching, including longer wait times, limited access to care, and potentially poorer health outcomes, particularly for those in rural and underserved communities. Addressing this crisis requires innovative solutions, such as telehealth, expanding the roles of nurse practitioners and physician assistants, and loan forgiveness programs to incentivize primary care specialization.
Resource Allocation: Bridging the Gaps
Significant gaps exist in resource allocation within primary healthcare. Millions lack access to a regular primary care physician, a problem exacerbated by rural hospital closures and the creation of “healthcare deserts.” Community health centers, often serving as a lifeline for underserved populations, are chronically underfunded and face challenges in maintaining consistent quality of care. Investing in these vital safety-net providers, promoting innovative models of care delivery like telehealth, and exploring strategies to incentivize primary care among medical students are crucial steps towards bridging these gaps and ensuring equitable access to care for all.
- Divided Food Storage Containers Transform Meal Prep and Portion Control - February 8, 2026
- Divided Food Containers Are Meal Preps Secret Weapon - February 7, 2026
- Food Kits for Adults Offer Fun DIY Cooking Adventures - February 6, 2026