Healthcare policy can be complex. This guide breaks down primary care policy in 2024, explaining the rules shaping your care, its cost, and its impact on community health. We’ll explore the key players, current challenges, and future directions of primary care, empowering you to navigate this vital aspect of healthcare.
Primary Care Policy: The Foundation of a Healthy Society
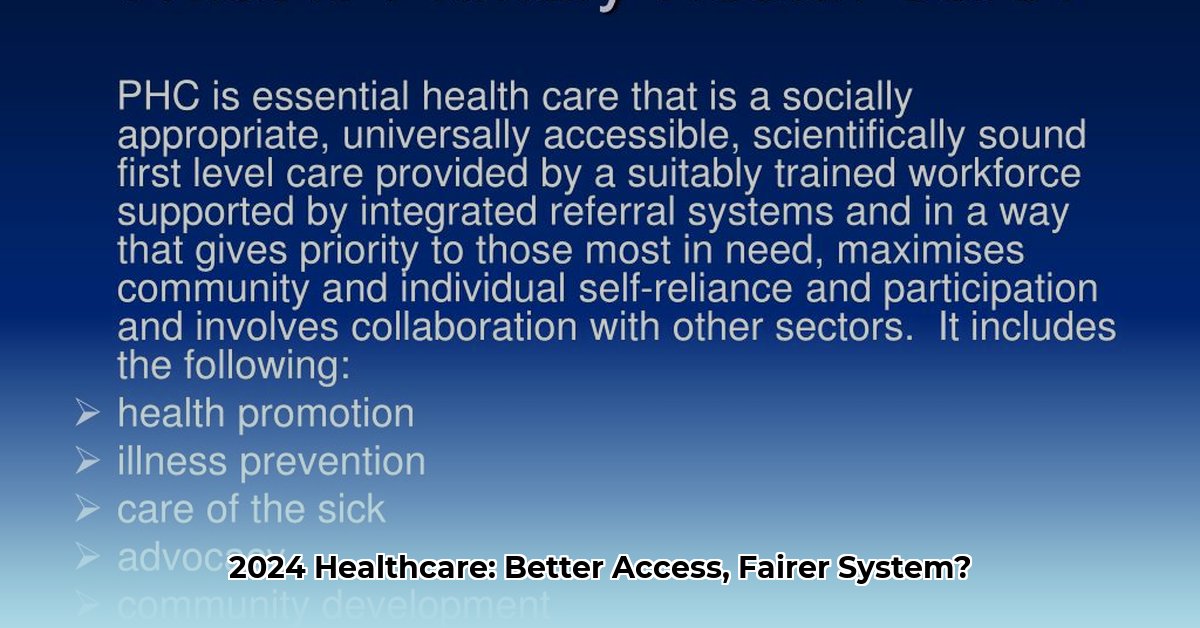
Primary health care policy sets the standards for essential healthcare services. These policies dictate access to check-ups, screenings, and vaccinations, impacting the availability and cost of care. A robust primary care system is fundamental to a healthy society, providing preventive care, chronic disease management, and health promotion, all of which contribute to broader goals like Universal Health Coverage.
Access: Ensuring Everyone Gets the Care They Need
A primary objective of primary care policy is equitable access for all, regardless of income or location. Strategies include establishing community health centers in underserved areas and expanding telehealth services. However, challenges persist, including healthcare professional shortages and geographic disparities in access, which policymakers continually address.
Equity: Tailoring Care to Individual Needs
Equitable care goes beyond treating symptoms. It requires considering the social determinants of health, such as access to nutritious food, stable housing, and education. These factors significantly influence a person’s overall well-being. Truly equitable primary care must account for these individual and community-specific needs.
Outcomes: Measuring the Effectiveness of Policies
Evaluating policy effectiveness involves analyzing data on health outcomes. Are people healthier? Are preventable hospitalizations decreasing? Is the system becoming more efficient? Organizations like the OECD and HRSA compile valuable statistics to assess the impact of policies and identify areas for improvement. Ongoing analysis helps refine strategies and optimize resource allocation.
The US Healthcare System: A 2024 Perspective
Current US policy emphasizes strengthening the foundation of the healthcare system. Programs like “Making Care Primary” aim to increase funding for community health centers and encourage collaborative care among healthcare professionals. While this represents progress, ongoing challenges demand continuous innovation and adaptation.
Global Lessons and the Future of Healthcare
The World Health Organization (WHO) champions primary healthcare as central to Universal Health Coverage. Learning from successful strategies in other countries can help the US move closer to a future where quality healthcare is accessible to everyone. Emerging technologies like telehealth and artificial intelligence offer exciting possibilities for transforming care delivery. Furthermore, new payment models like value-based care may improve efficiency and quality. Collaboration among policymakers, healthcare providers, and communities is crucial for shaping a future where primary care is accessible, equitable, and effective.
Inside “Making Care Primary” (MCP)
Launching in July 2024, the MCP model represents a significant shift in primary care delivery and payment. Its tiered structure accommodates providers with varying levels of experience with value-based care. This model incentivizes chronic disease management, care coordination, and addressing social determinants of health. By rewarding providers based on patient outcomes, MCP encourages a proactive, holistic approach to primary care. While its long-term impact remains to be seen, MCP likely represents a major step toward more effective and integrated care.
HHS: Leading the Charge in Primary Care
The Department of Health and Human Services (HHS) is investing heavily in primary care, adjusting payment structures, encouraging teamwork, and integrating behavioral health services into primary care settings. This integrated approach recognizes the crucial link between physical and mental well-being.
Congress: Addressing Key Healthcare Issues
In 2024, Congress is focused on healthcare affordability, aiming to increase drug pricing transparency and expand telehealth access, particularly for rural populations. Bipartisan support for strengthening the primary care workforce underscores its importance to the nation’s health.
The Road Ahead: Opportunities and Challenges
The policy changes in 2024 present both opportunities and challenges. The long-term impact on patients, providers, and the entire healthcare system will probably be significant. Continued research and evaluation are needed to assess the effectiveness of these changes.
| Policy Area | Key Changes in 2024 | Potential Impact |
|---|---|---|
| MCP Model | Tiered value-based care | May improve care coordination and outcomes |
| HHS Initiatives | Increased investments, team-based care | May enhance access and quality of care |
| Congressional Activity | Affordability focus | May improve access to affordable care |
Who Shapes Primary Care Policy?
Primary care policy is influenced by a dynamic interplay of stakeholders, each with distinct interests and levels of influence. Understanding these dynamics is crucial for navigating the healthcare system and advocating for effective policy changes.
Government: Setting the Stage
Government agencies at the federal (e.g., HHS) and state levels play a pivotal role. They establish regulations, control funding for programs like Medicare and Medicaid, and launch initiatives that shape care delivery.
Lobbying and Advocacy: A Powerful Force
Lobbying groups, representing various interests (pharmaceutical companies, hospitals, insurers), wield considerable influence on legislation. Patient advocacy groups and professional organizations also actively advocate for their constituents’ needs.
Research and Data: Informing Decisions
Think tanks and universities conduct research that informs policy decisions. Their analyses of policy effectiveness and healthcare trends provide evidence-based insights for shaping the future of primary care.
Healthcare Professionals and Patients: Frontline Perspectives
Doctors, nurses, and other healthcare professionals offer invaluable frontline perspectives on the challenges and opportunities in primary care. Patients are becoming increasingly vocal advocates for their own healthcare needs.
Media: Shaping Public Perception
The media plays a significant role in shaping public perception of healthcare issues. By highlighting challenges and successes, journalists and social media influencers can influence public opinion and policy decisions.
| Stakeholder Group | Influence | How They Impact Policy |
|---|---|---|
| Government Agencies | High | Funding, regulations, program development |
| Lobbying & Advocacy Groups | High | Legislative pressure, public campaigns |
| Think Tanks & Academia | Moderate to High | Research, data analysis, policy recommendations |
| Healthcare Professionals | Moderate | Expert testimony, advocacy |
| Patients | Increasing | Shared experiences, advocacy |
| Media | Moderate to High | Shaping public opinion |
Key US Primary Care Policies Explained
The US primary care landscape is shaped by a complex web of policies, impacting access, cost, and quality of care.
Insurance: Gateway to Care
Health insurance, whether Medicare, Medicaid, or private, is the primary gateway to primary care. The Affordable Care Act aimed to expand coverage, but challenges remain for uninsured and underinsured individuals.
“Making Care Primary”: A Novel Approach
As previously mentioned, the MCP model seeks to improve primary care by incentivizing value-based care, care coordination, and addressing social determinants of health. Its effectiveness will be closely monitored as it rolls out.
Provider Shortages: A Looming Crisis
Addressing the growing shortage of primary care physicians is crucial. Policies such as loan forgiveness programs, increased residency slots, and support for community health centers aim to attract and retain primary care providers.
Prevention: Investing in Long-Term Health
Greater emphasis on preventive care, including regular check-ups, vaccinations, and screenings, can improve health outcomes and potentially reduce long-term healthcare costs.
Health Equity: Striving for Equal Access
Achieving health equity requires policies that address disparities in access to quality primary care. Culturally competent care, language access, and expanding services in underserved communities are essential.
The Future of Primary Care: Innovation and Adaptation
The primary care landscape is constantly evolving. Telehealth, value-based care, and integrated mental health services are transforming how care is delivered. Policymakers must adapt to these changes to ensure equitable access, quality, and affordability.
The Impact of Policies on Access, Cost, and Outcomes
Policies directly impact access to primary care, its cost, and ultimately, health outcomes.
Access: Removing Barriers
Policies like funding for community health centers, insurance expansion, and telehealth initiatives can improve access to primary care. Addressing geographic disparities and ensuring that care is readily available are crucial.
Cost: Navigating the Complexities
Policies influence healthcare costs through reimbursement rates, payment models (fee-for-service versus value-based care), and prescription drug pricing regulations. The ongoing debate regarding cost containment versus quality of care requires careful consideration.
Outcomes: Measuring Success
The true measure of effective primary care policy is its impact on health outcomes, such as life expectancy, infant mortality, and chronic disease management. Data-driven analysis helps determine
whether policies are achieving their intended goals.
Striking a Balance: Cost vs. Quality
Balancing cost containment and quality care is an ongoing challenge. Investing in primary care may yield long-term cost savings by preventing costly hospitalizations and improving overall
population health.
The Future of Policy: Adapting to Change
The healthcare landscape is dynamic. Emerging technologies, evolving models of care, and a growing understanding of social determinants of health require ongoing policy adaptation to maximize primary care’s effectiveness and ensure a healthier future for all.
- Borosilicate Glass Food Containers Keep Meals Fresh and Organized - January 26, 2026
- Choosing Glass Containers With Snap Lids for Fresh Food Storage - January 25, 2026
- Borosilicate Containers Keep Food Fresh and Your Kitchen Organized - January 24, 2026