Healthcare can be complex, but it all begins with primary care. This guide serves as your roadmap to navigating the diverse landscape of primary health care models, from traditional doctor visits to innovative team-based approaches. We’ll explore the core components of each model, examining their benefits, drawbacks, and real-world examples. We’ll also delve into emerging trends like telehealth and value-based care, and discuss how these models strive to achieve health equity.
Decoding Primary Care: The Foundation of Health
Primary health care is the bedrock of a healthy life, encompassing much more than annual check-ups. It’s the first point of contact for medical needs, focusing on prevention, early detection, and ongoing management of chronic conditions. It’s the “front door” to the healthcare system, striving to keep you well and minimize the need for specialized or emergency interventions. Primary health care models are the organizational frameworks that define how this essential care is structured and delivered.
Navigating the Landscape: Types of Primary Care Models
Primary care models vary considerably, each with its own strengths and weaknesses. Understanding these distinctions helps us navigate the complexities of healthcare delivery and choose the right approach for individual needs. Let’s examine several prevalent models:
1. Physician-Centered Care: The Traditional Approach
This familiar model involves direct, one-on-one interaction between a patient and their physician. The doctor diagnoses and prescribes treatment, acting as the primary decision-maker. While effective for acute issues, this model may struggle with complex or chronic conditions requiring a multidisciplinary approach. Studies suggest this traditional model may sometimes lack care coordination, resembling different chefs preparing parts of a meal—delicious individually, but perhaps not a cohesive dining experience.
2. Team-Based Care: The Collaborative Approach
Team-based care involves a coordinated team of healthcare professionals, including doctors, nurses, pharmacists, social workers, and others. This collaborative approach aims to provide holistic patient care. This model probably fosters better communication and comprehensive care, particularly for individuals with chronic or complex needs. It’s like an orchestra, different instruments harmonizing to create a complete symphony of care.
3. Community Health Worker (CHW) Model: Bridging the Gap
CHWs are trusted members of their communities who link individuals to health services. They possess invaluable cultural understanding, serving as bridges between the healthcare system and underserved populations. CHWs act as guides, navigating complex healthcare landscapes for those who may otherwise face barriers to access.
4. Patient-Centered Medical Home (PCMH): Putting Patients First
The PCMH model prioritizes patient-centered care, emphasizing personalized, comprehensive, and coordinated services. The patient’s needs, preferences, and goals are central to the care plan. It’s like having a personalized health roadmap, guiding individuals through their healthcare journey. PCMHs strive to effectively manage both acute and chronic conditions.
5. Making Care Primary (MCP) Model: A New Era in US Healthcare
Launched in July 2024 by the Centers for Medicare & Medicaid Services (CMS), MCP aims to enhance primary care for Medicare beneficiaries. This model seeks to bolster care management, empower clinicians, and integrate community resources to address social determinants of health. MCP utilizes a three-track system, catering to varying levels of experience with value-based care.
Here’s a breakdown of MCP’s key features:
| Feature | Description |
|---|---|
| Goal | Improve care management, empower primary care clinicians, leverage community connections to address health and social needs. |
| Duration | 10.5-year initiative. |
| Participating States | Colorado, North Carolina, New Jersey, New Mexico, New York, Minnesota, Massachusetts, Washington. |
| Tracks | Three distinct tracks for varying levels of value-based care experience. |
| Payments | Blend of fee-for-service and prospective, population-based payments (track-dependent). Enhanced services payments for care management and integration. |
| Eligibility | Legal entity serving ≥125 Medicare beneficiaries with a majority of sites in MCP states. Excludes Rural Health Clinics, concierge practices, current PCF practices, current ACO REACH Participant Providers, and Grandfathered Tribal FQHCs. |
| Focus Areas | Care management, specialty integration, addressing social determinants of health. |
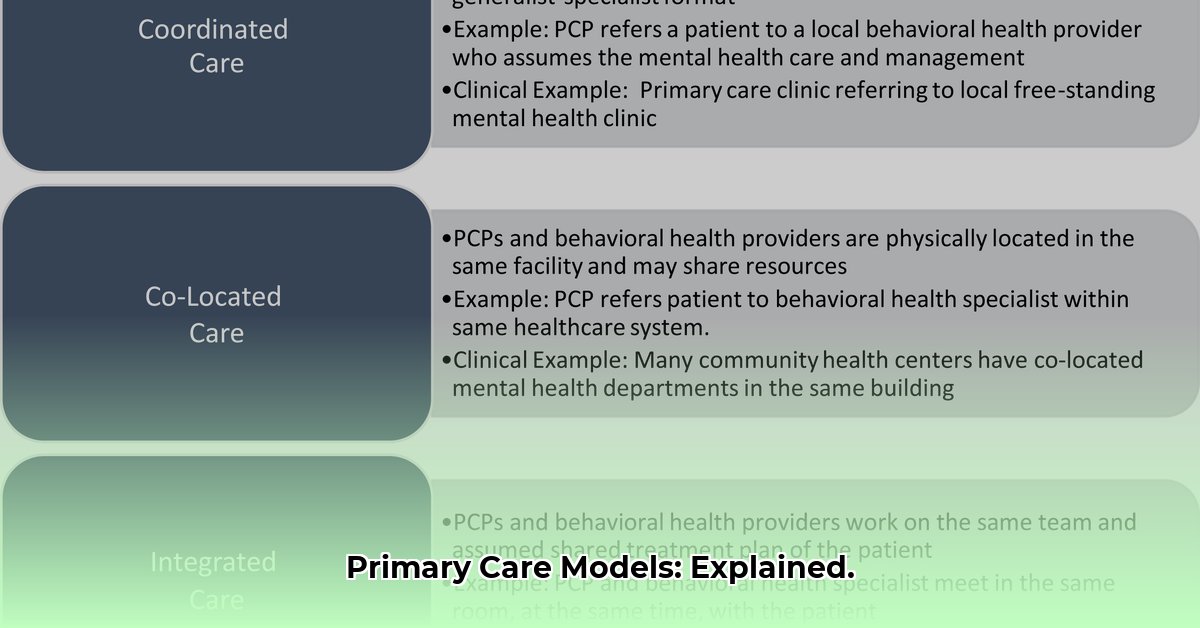
6. Integrated Care: A Holistic Approach
Integrated care acknowledges the interconnectedness of physical and mental health with social well-being. It combines medical and social services, addressing factors like housing and food security. This evolving approach recognizes that factors outside the clinic significantly impact overall health. Early research suggests promising results, but further study is necessary to fully determine the long-term effects.
Essential Elements of Successful Models
Effective primary care models typically share these fundamental characteristics:
- Accessibility: Ease of scheduling appointments and accessing required services.
- Affordability: Cost-effectiveness for both patients and the healthcare system.
- Patient-Centeredness: Prioritizing patient preferences, experiences, and empowerment.
- Quality: Delivery of evidence-based care leading to positive health outcomes.
- Coordination: Seamless care coordination between diverse providers and specialists.
- Equity: Addressing health disparities and promoting equitable access for all, regardless of background.
The Future of Primary Care: Embracing Innovation
Primary care is constantly adapting to advancements in technology and evolving patient needs. Telehealth is becoming increasingly prevalent, expanding access, particularly for those in rural or underserved areas. Remote patient monitoring, artificial intelligence, and other technologies promise more personalized and proactive care. These innovations hold the potential to further transform healthcare delivery, though careful consideration of data privacy and equitable access to technology is crucial.
Health Equity: A Fundamental Principle
Health equity is a cornerstone of successful primary care. Every individual, regardless of background or circumstance, deserves access to quality care. Primary care models must actively address disparities and strive to achieve health equity, ensuring everyone can achieve their optimal health.
Implementation: A Roadmap for Change
Implementing new primary care models requires careful planning, resource allocation, and a commitment to continuous improvement. It’s a complex process demanding collaboration among stakeholders and ongoing evaluation to adapt to evolving needs.
Python and Primary Care Modeling: A Data-Driven Approach
Python, a powerful programming language, offers valuable tools for analyzing, modeling, and optimizing primary health care delivery. Libraries like PyHealth, APLUS, SimPy, SciPy, NumPy, and Pandas provide resources for building simulations, predicting disease spread, optimizing resource allocation, and modeling patient flow. These data-driven insights can inform decision-making and enhance the effectiveness of primary care interventions.
Conclusion: A Path to Better Care
Understanding the diverse landscape of primary health care models is essential for building a more effective and equitable healthcare system. This evolving field demands continuous exploration, innovation, and a steadfast commitment to patient-centered care. By embracing new technologies, prioritizing health equity, and fostering collaboration, we can pave the way for a healthier future for all.
- Borosilicate Glass Food Containers Keep Meals Fresh and Organized - January 26, 2026
- Choosing Glass Containers With Snap Lids for Fresh Food Storage - January 25, 2026
- Borosilicate Containers Keep Food Fresh and Your Kitchen Organized - January 24, 2026